Background Information
Rates of Reaction
Collision Theory
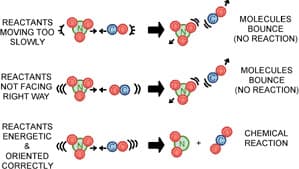
The collision theory explains why chemical reactions take place. The theory is based on the assumption that for a chemical reaction to happen, reacting particles must collide. However, even if the particles collide, there is still a chance a reaction will not take place because the reacting particles must have a specific orientation when they collide. For example, consider the formation of NO2 and CO2 from NO3 and CO. The two reactant molecules will react only if they have the proper orientation: that is, the N of NO3 molecules must collide with the C of CO molecules. This is shown in figure 1 6 below.
Despite having the right orientation, reacting particles will not form products if they do not have the necessary minimum amount of energy needed for the reaction to happen. This minimum amount of energy is called activation energy. As Figure 2 shows, think of activation energy as the hill that the reactants must overcome in order to be changed into products. A higher hill means a higher activation energy.
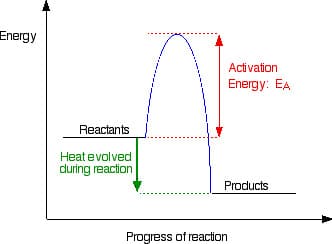
In summary, the collision theory tells us that three conditions are needed for a reaction to occur. First, the reactants must collide. Second, the reactants must collide in a specific orientation. Finally, reactants must possess a certain minimum amount of energy called activation energy upon collision so that they will be changed into products.
Factors affecting Reaction Rate
Four factors that affect how fast a reaction will happen include concentration, temperature, surface area, and presence of a catalyst. How each factor speeds up or slows down a reaction can be explained in terms of the collision theory.
An increase in the concentration of the reactants speeds up the reaction. A higher concentration means there are more reacting particles per volume, which increases the frequency of collisions and, hence, the rate of reaction.
Increasing the temperature increases the kinetic energy of the reacting particles. This causes the particles to move faster and collide more frequently. At the same time, increasing the temperature also means more particles have the activation energy needed for the reaction to take place.
Smaller pieces of firewood burn faster than a big log of wood. The material available for burning is the material at the surface of the log: therefore, because smaller pieces of wood have a larger surface area per volume than a big piece of wood, they burn faster. Increasing surface area increases the number of reaction sites. Consequently, the frequency of effective collisions increases and the reaction happens faster.
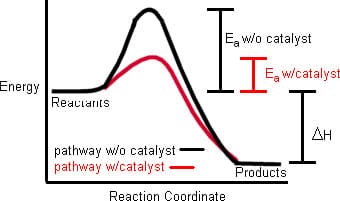
Many reactions will occur faster with the use of catalysts. A catalyst is a substance that speeds up a reaction without itself being consumed in the reaction. For example, hydrogen peroxide decomposes slowly into water and oxygen. Adding potassium iodide speeds up the reaction. But potassium iodide is not used up in the course of the reaction, so it can be used over and over again.
A catalyst speeds up a reaction by lowering the activation energy as shown in Figure 3 below. Note how the initial and final energy of the system remain the same with or without a catalyst but the pathway of a catalyzed reaction shows a lower energy ""hill"", making it easier for the reactants to be converted into products. Think of the lower hill as a tunnel dug into a mountain. Instead of going up the hill to cross to the other side, cars can just pass through the tunnel and get to the other side faster.
Enzymes
Many chemical reactions taking place in the cells of living organisms require a catalyst. These biological catalysts are called enzymes. Enzymes are proteins that speed up almost all vital chemical reactions that would otherwise take place very slowly or not happen at all, thus compromising the organism''s survival. For example, the enzyme amylase is found in human saliva. Amylase speeds up the conversion of starch into sugar. Amylase is also found in the pancreas where it is used to break down carbohydrates.
Hydrogen peroxide bubbles when poured onto a cut or wound. The enzyme catalase is found in many cells throughout the body. Catalase breaks down hydrogen peroxide into water and oxygen. The bubbles observed are actually the oxygen produced. Hydrogen peroxide does not bubble when it comes into contact with unbroken skin because the catalase has not been released.
Enzymes are very specific when it comes to catalyzing biochemical reactions in organisms. The substrate or substance that will be converted into the product requires a particular enzyme. Only when the substrate fits the enzyme like a key in a lock can the biochemical reaction occur.
Like all other proteins, enzymes are polymers of hundreds (and even thousands) of amino acids. Each enzyme has a unique sequence of amino acids. No two enzymes have the same sequence of amino acids. A simple change in the sequence drastically alters the ability of an enzyme to catalyze a biochemical reaction.
The sequence of amino acids in enzymes forms coils and folds that result in a three–dimensional structure. Only a small part of this three–dimensional structure, called the active site, interacts with the substrate during the biochemical reaction. The active site complements the shape of the substrate that will be converted into another substance. If the shapes don''t fit, biochemical reactions will not take place.
Some substances prevent enzymes from interacting with the substrate. These substances are called enzyme inhibitors. Drugs and poisons often have their biological effects because they are enzyme inhibitors.
How We Sense Pain
The Pain Pathway
The most widely accepted definition of pain comes from the International Association for the Study of Pain which defines pain as ""an unpleasant sensory and emotional experience arising from actual or potential tissue damage or described in terms of such damage"" 7. Pain as a subjective, psychological experience is a necessary element to our survival because it tells us to avoid potentially harmful events and to protect damaged tissue while it heals.
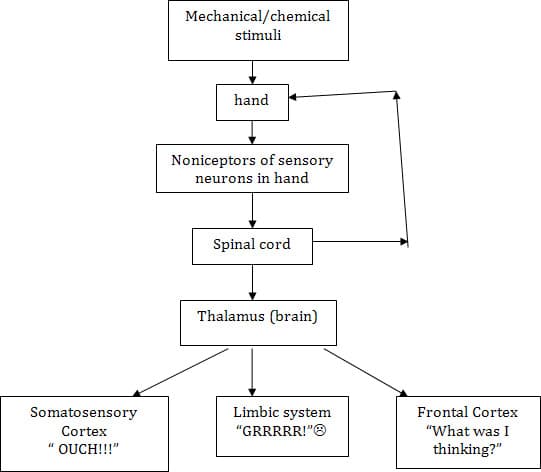
But how do we sense pain? The process by which a painful stimulus is transmitted to the central nervous system is called nociception. A simple description of this process involves the following steps 8:
- A mechanical or chemical stimulus that damages or could potentially damage tissue occurs. A mechanical stimulus can be pressure (like stubbing your toe), a puncture, or cut. A chemical stimulus includes burns.
- Sensory neurons with specialized receptors or nerve endings sensitive to pain stimuli detect the stimulus. Neurons with these special pain receptors called nociceptors are found in the skin, internal organs, joints, muscles and tendons.
- Nociceptors transmit the pain signal to the spinal cord and brain.
- The brain receives the signal for processing and action.
For example, when you pick up the hot lid of a cooking pan with your bare hand, nociceptors in your fingers, detecting the heat, send an impulse through a sensory neuron to your spinal cord. Recall that the spinal cord relays all kinds of impulses to and from the brain. At the same time, the spinal cord also has the ability to make decisions on its own called reflexes. The impulse is received by an area of the spinal cord called the dorsal horn which does two things at the same time. The dorsal horn relays an immediate message—through a reflex arc that connects the sensory neuron to motor nerves that connect to muscles in the injured fingers—to pull away and you drop the hot object. This is an automatic, involuntary reflex, which the brain does not have to order.
At the same time , the dorsal horn relays the pain signal to an area of the brain called the thalamus. The thalamus acts like a sorting station that evaluates signals and sends them to appropriate areas of the brain for interpretation. The pain signal is sent to the somatosensory cortex (responsible for physical sensation), the frontal cortex (in charge of thinking), and the limbic system (linked to emotions) 9. As a result, you feel the sensation of pain in your hand, you think picking up the hot lid without using a pot holder was a ""silly"" thing to do, and react emotionally by feeling annoyed at yourself for your lack of common sense. At the same time, the pain signal can also stimulate parts of the brain that control an increase in blood pressure, heart and breathing rate.
Figure 4 below shows a simple flowchart of the pain pathway.
Classifying Pain
There are different ways to classify pain. One form of classification divides pain into two main categories: nociceptive pain and non–nociceptive pain 1 0. Nociceptive pain involves the stimulation of nociceptors that respond to heat, cold, pressure and chemical stimuli released by damaged cells. Non–nociceptive pain, on the other hand, results from a malfunction of the peripheral or central nervous system. No specific nociceptors are stimulated. A good analogy to consider in distinguishing between the two types of pain is a fire alarm. A fire alarm set of by smoke represents nociceptive pain while a fire alarm that goes off simply because it has malfunctioned is non–nociceptive pain.
Nociceptive pain may be further classified into two sub–types: somatic and visceral. Somatic pain involves the stimulation of nociceptors found in the tissues of skin, muscles, joints, bones, and ligaments. Heat, cold, vibration, stretch (muscles), inflammation (e.g. cuts and sprains which cause tissue disruption), and oxygen starvation (muscle cramps) are stimuli that activate these nociceptors. The pain is sharp and localized and touching or moving the damaged area reproduces the pain. Visceral pain results from the stimulation of nociceptors found in the internal organs of the three main cavities which include the heart and lungs in the thorax, liver, kidneys, spleen and bowels in the abdomen, and the bladder, womb, and ovaries in the pelvis. Pressure, inflammation and oxygen starvation are the stimuli that produce this type of pain which ""is poorly localized, and may feel like a vague deep ache, sometimes being cramping or colicky in nature"" 1 1. It usually produces referred pain (pain felt at a site other than where the source is located) to the back, with pelvic pain referring pain to the lower back, abdominal pain referring pain to the mid–back, and thoracic pain referring pain to the upper back"" 1 2.
Non–nociceptive pain is either neuropathic or sympathetic. Neuropathic pain, also known as pinched or trapped nerve, stems from mechanical problems within the nervous system itself, either from the nerves between the tissues and the spinal cord (peripheral nervous system) or from the nerves between the spinal cord and the brain (central nervous system). The pain sensation arises from damage to the nerves due to degeneration such as in multiple sclerosis, pressure resulting in a trapped nerve, inflammation due to a slipped disc or a viral infection like shingles 1 3. The damaged nerve fires off pain signals in a random and chaotic manner.
Sympathetic pain may be caused by over–activity of sympathetic nervous system, and central / peripheral nervous system mechanisms which could arise from fractures and soft tissue injuries of the arms and legs. This type of pain is associated with extreme hypersensitivity in the skin around the injury and also peripherally in the limb and even excessive sweating and increased temperature in the damaged area because blood flow, which is controlled by the sympathetic nervous system, is erratic 1 4. The limb is usually so painful, that the patient refuses to use it, causing secondary problems after a period of time with muscle wasting, joint contractures, and osteoporosis of the bones 1 5.
Biosynthesis of Prostaglandin By Arachidonic Acid Pathway
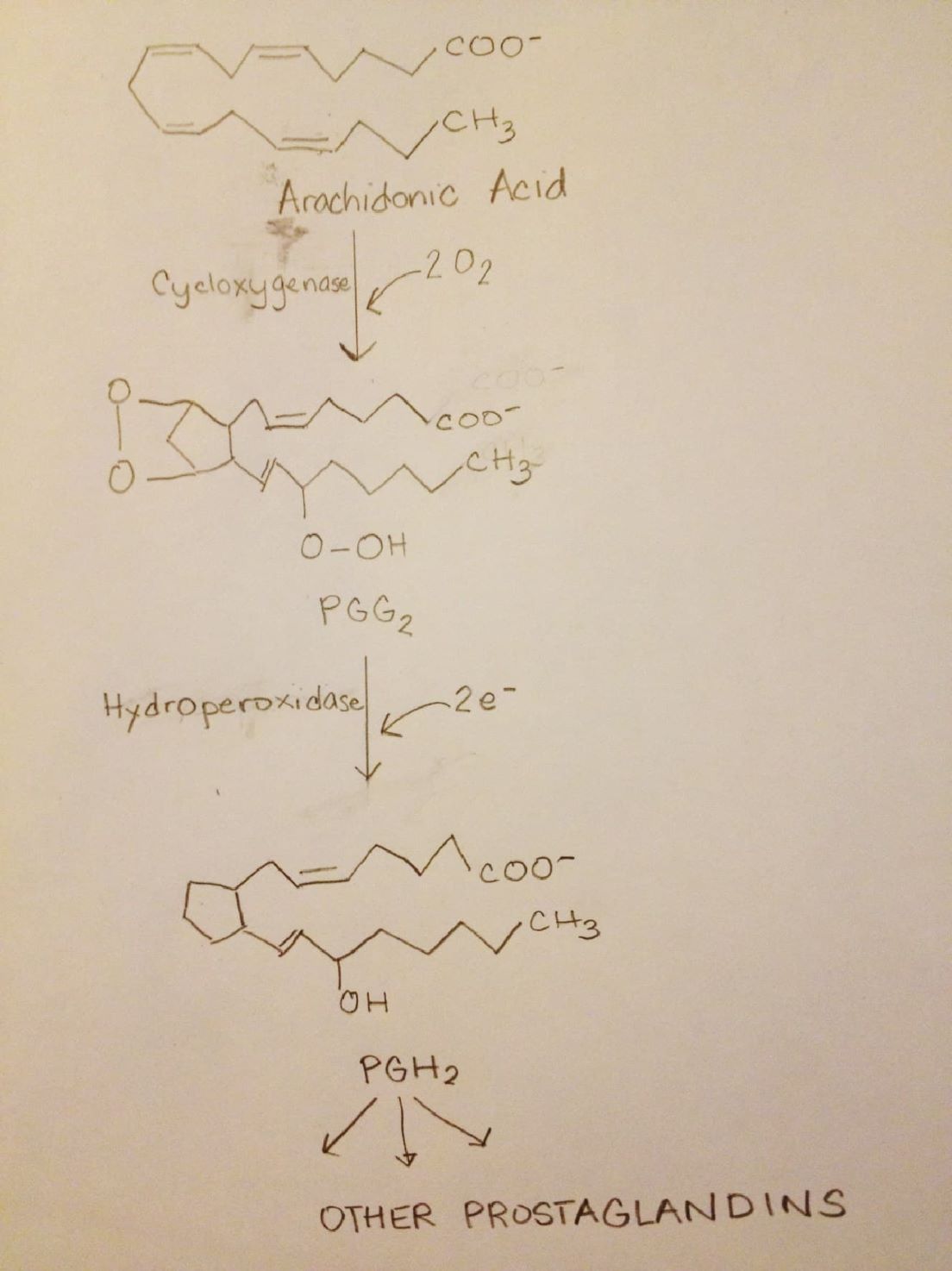
The synthesis of prostaglandin in the body starts when physical, chemical, and inflammatory stimuli including tissue damage activate an enzyme called phospholipase A2. This enzyme produces a fatty acid called arachidonic acid using membrane phospholipids as the substrate. Arachidonic acid is then metabolized to other substances, one of which is prostaglandin.
A complex enzyme called prostaglandin synthase catalyzes the conversion of arachidonic acid to the first prostaglandin PGG2 . This enzyme is also known as cyclooxygenase or COX because it adds oxygen and forms a ring. A different active site of the enzyme COX is then used to change PGG2 to another prostaglandin PGH2 . Since the reaction involves the reduction of a hydroperoxyl in PGG2 to a hydroxyl in PGH2 , the enzyme in this step is called hydroperoxidase. The action of other enzymes then converts PGH2 to various physiologically active prostaglandins. Figure 5 1 6 shows this prostaglandin synthesis pathway.
Physiological Activity of Prostaglandin
Prostaglandins mediate a variety of physiological processes. Elevated concentrations of prostaglandin—which are produced by higher rates of synthesis due to the enzyme systems described above—trigger an inflammatory response which is the body''s way to counter the infection resulting from tissue damage. Inflammatory response includes fever, swelling and pain. Pain occurs because nociceptors are sensitive to changes in prostaglandin concentration. An increase in the synthesis of prostaglandin stimulates noniceptors and the pain pathway described above begins.
Prostaglandins are involved in more than the creation of local pain. Prostaglandins found in blood platelets can be converted to thromboxanes which are powerful blood clotting agents. Prostaglandins in the gastrointestinal tract are involved in lessening gastric acid and increasing mucus secretion. Certain prostaglandins are involved in many stages of reproduction including the normal implantation of the fertilized oocyte, induction and initiation of labor. For example, PGE2 causes uterine contraction and hence menstrual cramps. It also has been used as a drug to induce labor.
Prostaglandins are involved in control of blood vessel constriction and dilation. Individuals with compromised kidneys because of one or more chronic organ diseases need prostaglandin in their kidneys to facilitate smooth renal flow. Other prostaglandins regulate blood pressure. Some prostaglandins promote the constriction of bronchi associated with asthma.
In the early 1990''s, several investigations showed that humans and other mammals have two genes for COX, the key enzyme in prostaglandin synthesis from arachidonic acid. These isoforms of the enzyme are called COX–1 and COX–2. Though they have very similar structures, they differ in terms of substrate, inhibitor selectivity and location within the cell. COX–1, found in most tissues, is called a housekeeper enzyme 1 7. It helps maintain homeostasis in many organs. For example, the prostaglandins involved in blood clotting, gastric mucus secretion and smooth renal flow in compromised kidneys are synthesized by COX–1.
On the other hand, COX–2 is inducible by inflammation 1 8. Prostaglandins resulting from the action of COX–2 are associated with inflammation, fever, pain, ovulation and the birth process. Both COX–1 and COX–2, though, have the same affinity for arachidonic acid so either isoform can catalyze the first two steps in the arachidonic acid pathway for prostaglandin synthesis.
Over-The-Counter Pain Relievers
There are two kinds of over–the–counter (OTC) pain relievers, nonsteroidal, anti–inflammatory drugs (NSAIDs) and acetaminophen (also known as paracetamol). NSAIDs include aspirin, ibuprofen, and naproxen.
Aspirin
One of the most versatile drugs ever produced is aspirin or acetylsalicylic acid. It is an analgesic (i.e. it relieves pain), anti–pyretic (i.e. it reduces fever), and anti–inflammatory (i.e. it prevents swelling, redness and other symptoms associated with inflammation). It has also been prescribed for the prevention of stroke and heart attack.
Aspirin owes its origin to the ancient practice of using willow bark extract to ease pains and reduce fever. In fact, the father of modern medicine Hippocrates wrote about a bitter powder that could be extracted from willow bark and could be used as pain and fever remedy. By the early 1880''s, it was known that the active ingredient was salicin, which is transformed to salicylic acid once it is ingested. Figure 6 below is the structure of salicylic acid.
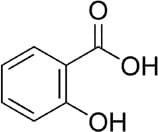
Salicylic acid was first synthesized from salicin by Italian chemist Raffaele Piria in 1838. In 1859, Adolph Kolbe working with other chemists at the Bayer Company in Germany, synthesized salicylic acid by heating phenol with carbon dioxide. But salicylic acid is such a stomach irritant that ""many patients preferred their aches and fever to the severe heartburn caused by the remedy."" 1 9
In 1899, Felix Hoffman, a junior chemist at Bayer Company who was on the lookout for an alternative medication for his father suffering from severe arthritis, modified salicylic acid to make it more soluble in stomach acid and thus make it pass through the stomach faster. He reasoned that this chemical change would make the drug less irritating to the stomach. He came up with acetylsalicylic acid with a chemical formula of C9 H8 O2 . Bayer named the new drug aspirin: a from acetyl, and spirin from spirea or meadowsweet flower which is one of the natural plant sources of salicylic acid.
Acetylsalicylic acid is a weak acid that can go through the mucus lining of the stomach. The upper portions of the small intestine absorb most of the drug. It breaks down into acetic acid and salicylic acid once it enters the bloodstream. The structure of acetylsalicylic acid is shown in Figure 7.
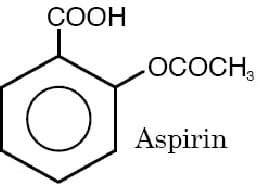
Though aspirin is more soluble in stomach acids, it can still cause stomach irritation in a small percentage of people. For that reason, there is buffered aspirin which is made by combining the aspirin with an acid buffer thus reducing acidity. Still, stomach irritation is a major problem for people such as those suffering from arthritis who have to take aspirin daily. These people can take specially coated aspirin tablets that pass through the stomach without dissolving. Acids in the stomach are unable to dissolve the coating but the basic environment in the small intestine quickly disintegrates it.
How is aspirin able to accomplish a variety of functions? Aspirin works by inhibiting the COX enzyme, which sits at the start of the arachidonic acid pathway for the synthesis of prostaglandins, thus stopping the synthesis of prostaglandin. In 1994, a group of researchers from the University of Chicago figured out the molecular structure of the enzyme. Using X–rays to probe the positions of the atoms in tiny crystals of the enzyme, they found out that the ""enzyme has a tunnel running into the middle of it. The substrate arachidonic acid must pass through this tunnel to reach the core of the enzyme, where it will be converted into prostaglandin"". 2 0
In 1995, the same researchers reported that ""aspirin permanently attaches a portion of itself inside the tunnel, where it acts as a gate, blocking prostaglandin''s precursor from reaching the active site of the enzyme. They also showed that this gate can be in two positions, either fully or partially closed, and that the position of the gate may differ between the two forms of the enzyme, COX–1 and COX–2."" 2 1 Other investigations show that aspirin permanently inhibits the enzyme because it forms a strong covalent bond with the enzyme which cannot be broken. 2 2 This is an example of irreversible inhibition.
The ability of aspirin to bind with COX–2—which is responsible for the synthesis of prostaglandins associated with pain, fever and inflammation—explains why the drug is an analgesic, antipyretic, and anti–flammatory. Since it also inhibits COX–1 associated with the production of prostaglandins responsible for basic housekeeping duties such as increasing mucus secretion to protect the gastrointestinal tract, aspirin produces side effects such as stomach upset, gastric ulcers, and gastric bleeding.
Furthermore, aspirin helps prevent stroke because inhibiting COX–2 limits the synthesis of prostaglandins that mediate platelet aggregation and blood clotting. A stroke could result from a blood clot blocking flow in smaller blood vessels in the brain, resulting in oxygen deficiencies. Some people refer to aspirin as a ""blood thinner."" This is not really an accurate description since what aspirin does is to stop the formation of prostaglandins that make platelets in the blood ""stick together"" and produce blood clot.
Ibuprofen
Ibuprofen is an NSAID drug marketed under various names including Advil and Motrin. It was developed and discovered by a team that was part of the research arm of the Boots company in the United Kingdom in the 1950s, patented in 1961, and first made available under prescription in 1969. 2 3 It became available in the United States in 1974 as a prescription drug and an OTC drug in 1984. 2 4
Though it has antipyretic and anti–inflammatory properties, ibuprofen is widely marketed as an analgesic. It is particularly known for providing relief from arthritis and is widely used for the relief of headache including migraine and other pain conditions arising from various injuries especially those that involve inflammation, illnesses such as influenza and post–operative pain. It is also used to relieve the symptoms of primary dysmenorrhea.
The chemical name of ibuprofen is 2–(4–isobutylphenyl)propanoic acid. It has a molecular weight of 206.3. Its empirical formula is C1 3 H1 8 O2 and its structural formula is shown by Figure 8.
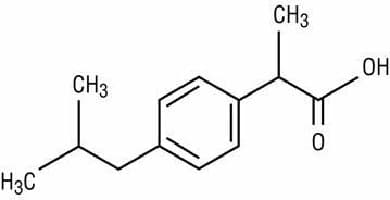
Ibuprofen and aspirin have analogous functions but lower doses of ibuprofen produce less irritation of the gastrointestinal tract.
The mechanism of action of ibuprofen is similar to aspirin. It also inhibits COX at the beginning of the arachidonic acid pathway thus shutting down prostaglandin synthesis. Just like aspirin, it also inhibits both COX–1 and COX–2, but ibuprofen acts on the enzymes in a slightly different way. Ibuprofen forms a noncovalent bond with the enzyme. 2 5 This bond is not as strong as the bond formed by aspirin with COX. When the bond eventually breaks, the enzyme becomes active again. Ibuprofen is thus considered a reversible inhibitor.
Naproxen
Naproxen is the active ingredient of the OTC NSAID Aleve. It is the most recent of the four most popular OTC analgesics sold in the United States. 2 6 It is also available as a sodium salt, naproxen sodium, which is more rapidly absorbed from the gastrointestinal tract. 2 7 It is commonly used for the reduction of mild to moderate pain, fever, inflammation and stiffness caused by conditions such as arthritis, gout, menstrual cramps, tendinitis and primary dysmenorrhea. 2 8
Naproxen was developed by the Syntex drug company in 1976. It was first sold as a prescription drug under the name Naprosyn. It quickly became the leading arthritis drug in the United States giving Syntex 80% gross profit margins. 2 9 Naproxen sodium was initially available as the prescription drug Anaprox in 1980. In 1994, the Food and Drug Administration approved naproxen sodium as an OTC drug.
Naproxen is an odorless, white to off–white crystalline substance with a molecular weight of 230.2628. 3 0 Its chemical name is (S)–6methoxy–αΑ–methyl–2–naphthaleneacetic acid and has an empirical formula of C1 4 H1 4 O3 . Its structural formula is shown by Figure 10. 3 1
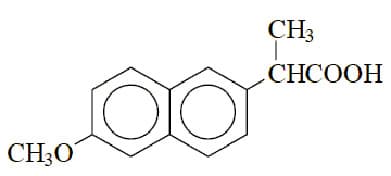
It is nonpolar, which means it is soluble in lipids but almost insoluble in water with a pH below 4 but becomes readily soluble at pH 6 or higher. 3 2
Like aspirin and other NSAIDs, naproxen blocks the production of prostaglandins by inhibiting COX at the start of the arachidonic acid pathway, causing gastrointestinal tract irritation. Taking naproxen with food is one way to minimize this side effect.
Acetaminophen
Acetaminophen is found in several OTC medications such as Tylenol, Excedrin, Theraflu, and Nyquil as well as in prescription pain medicine like Vicodin which contains acetaminophen and another substance called hydrocodone. Though it was discovered by Harmon Northrop Morse in 1873, the medical use of acetaminophen began only in 1893. 3 3 It was approved for use by the U.S. Food and Drug Administration in 1950 3 4 and went on sale as Tylenol in 1955.
The chemical formula of acetaminophen is C8H9NO2. Its chemical name is 4–hydroxyacetanilide. Figure 11 shows its chemical structure:
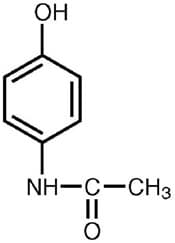
Like NSAIDs, acetaminophen is an analgesic and antipyretic. It has similar pain–relieving potency as aspirin and ibuprofen. But unlike NSAIDs, it does not possess anti–inflammatory properties. Thus, it cannot reduce the swelling of tissues resulting from a sprain or arthritis, for example.
Acetaminophen is an alternative for people who are allergic to aspirin. Because it does not stop mucus production, it causes less irritation to the gastro–intestinal tract and can be taken by those suffering from acid reflux and peptic ulcers. But unlike aspirin, it does not inhibit platelet aggregation therefore it does not provide reduced blood clotting protection for those who have heart problems.
Why does acetaminophen produce some similar effects as NSAIDs but also behaves differently? Just like NSAIDs, acetaminophen interferes with the synthesis of prostaglandins, hence, it relieves pain and reduces fever. But NSAIDs block prostaglandin synthesis at the beginning of the arachidonic acid pathway by binding with COX in the very first step, thus stopping the entire prostaglandin synthesis process. Consequently, all the physiological activities that involve prostaglandin are reduced including relay of pain signal, inflammation, fever, mucus production and blood clotting.
On the other hand, acetaminophen does not inhibit COX at the beginning of the pathway but another enzyme located further downstream. 3 5 At that juncture of the pathway, the synthesis of prostaglandins responsible for inflammation, mucus secretion and blood clotting has been completed. Moreover, it is believed that acetaminophen is much more specific in terms of where it inhibits prostaglandin production. It blocks prostaglandin synthesis more specifically in the tissues of the central nervous system whereas NSAIDs act on a broader range of tissues. 3 6 Some scientists believe acetaminophen inhibits a third form of COX called COX–3 found in the central nervous system but this is still subject to debate. 3 7
Acetaminophen is a safe and effective pain reliever as long as it is taken in its therapeutic dose of 500 mg every 4–6 hours. But it can severely damage the liver and even cause death when it is misused or abused. In fact, the improper use of acetaminophen has become the leading cause of acute liver failure in the United States. Enzymes in the liver break down acetaminophen into a very toxic compound called N–acetyl–p–benzoquinonimine. The body can easily detoxify and excrete small amounts of this compound. But when large amounts of the compound accumulate, the body''s detoxification system is overwhelmed and the compound starts killing liver tissues.

Comments: