Background
The global history of the common cold
The cold can be dated back to the Stone Age on the assumption that, with people living in such close proximity, it must have been present. Throughout China and Egypt, many herbal remedies and even acupuncture therapies were attempted to cure the cold once caught. During the Greco-Roman Era, many believed the cold was derived from the weather. In these settings, it was considered possible to burn the cold out to rid the body of mucus believing it was the cause of illness. Today, we know that mucus membranes line the mouth, nose, throat, sinuses, and lungs. These membranes can also be found lining the respiratory tract for protection and support. Think of it as the lid of a pot, holding the moisture in. It also contains antibodies that recognize the body’s invaders.
From the Early Modern Period to the 18th Century, plants became more of a regular remedy to remove the mucus from the brain or blood. In the 19th Century, proponents of the infection theory first associated the pathological microbes that caused illness with bacteria or simply called them “cold pathogens.”6 In 1946 the Common Cold Unit (CCU) was established shortly after the British began to warn the public of the danger of spreading infection and the importance of personal hygiene. “For about 50 years, we have known the culprits to be rhinoviruses or other subgroups of the so-called picornaviruses, which lead to short-lived infections in the mucus membranes of the nose, throat and sometimes the bronchial tubes.”7 Today, the common cold is still common and even more widespread than it has been in the past. There has been a discovery of a third emerging strand in recent years.
Respiratory system
To best understand the effects of an infection to the body, we must look at the system where the infections take place: the respiratory system. Like any body system, the respiratory system is comprised of a specialized group of organs. The system can also be divided into two different subgroups of organs, determining the upper and lower respiratory tracts. Together, these organs carry out multiple functions for living, but mainly facilitate the efficient trading of gases from the air to blood. Organ structures will be referred to as well as the range of functions are discussed that relate to this unit and previous units taught. Note that although cardiovascular system works closely with the respiratory system it will not be extensively discussed.
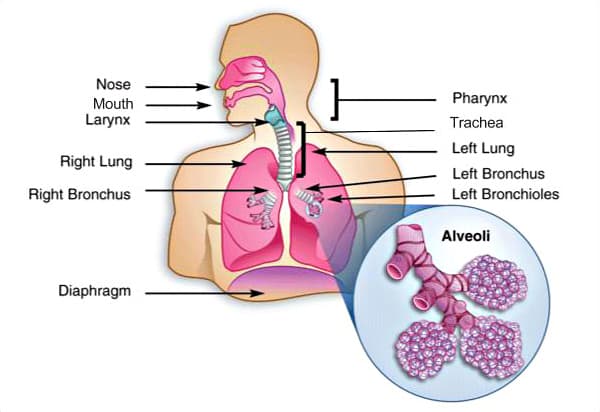
Figure 1 The structures of the human respiratory system. Courtesy: Diagram of "Human Lungs" Wikimedia Commons (public domain)
The respiratory system aids in breathing. While breathing, air is inhaled through the nose and mouth. Air then moves through the pharynx, larynx, and trachea into the lungs. When air is exhaled, it follows the same route as during entry but backwards. During typical inhalation, the diaphragm and chest walls contract, elevating the rib cage. During normal exhalation, the muscles relax. Gas exchange between the lungs and bloodstream is known as external respiration (Figure 1). Oxygen is exchanged for carbon dioxide waste inside the lungs through a process called external respiration. This respiratory process takes place through hundreds of millions of microscopic sacs called alveoli. Oxygen from inhaled air diffuses from the alveoli into pulmonary capillaries surrounding them. While pumping through the bloodstream, oxygen binds to hemoglobin molecules in red blood cells. Concurrently, carbon dioxide from deoxygenated blood diffuses from the capillaries into the alveoli, and is expelled through exhalation. The fluid in the bloodstream transports oxygen to cells and removes waste carbon dioxide through internal respiration, another essential function of the respiratory system. In this process red blood cells carry oxygen soaked up from the lungs around the body. When oxygenated blood reaches the narrow capillaries, the red blood cells free the oxygen. It diffuses through the capillary walls into body tissues. Simultaneously, carbon dioxide diffuses from the tissues into red blood cells and plasma. The deoxygenated blood carries the carbon dioxide back to the lungs for release.8
Respiratory Infections
Respiratory infections account for more than 4 million deaths annually and are the leading cause of death in developing countries. Since these deaths are preventable with adequate medical care, a much higher proportion of them occur in low-income countries.9 The respiratory tract can be categorized between two sections, the upper and lower tract. When considering an upper respiratory tract infection (RTIs), this would affect the nose, sinuses, and throat, for example the common cold or the flu. On the other hand, a lower respiratory infection affects the airways and lungs, pneumonia or the flu are examples of lower RTIs. Respiratory infection is caused by two different microscopic matters, bacterial or viral. Most infections are caused by viruses. Focusing on the rhinovirus, the common cold, I explore some characteristics of viruses, expanding on their structure and function, the various types, and how they replicate, hijacking your cells. Later, rhinovirus will be discussed and then further compared to the Influenza virus.
Viruses
Viruses were first visibly seen in 1931 when the electron microscope was invented. Viruses are not living and are smaller than bacteria. They are considered to be non-cellular replicators, containing genetic material. In order to replicate they need a living host. You may be asking yourself, “wait they’re not living but have genetic material like I do?” I had the same thoughts, hopefully I can make sense of this for you, as I did myself. Viruses can be classified by two different components, their genetic material and their capsid. All viruses include genetic material, but the details can vary: double-stranded DNA or single- or double-stranded RNA, and a protein coat (capsid), protecting the viral genome. If the virus contains DNA, the virus must enter into the cells nucleus where its DNA is housed, with the ability to directly inject its DNA into the host cells’ nucleus. Viruses get really slick when they have RNA. They must trick the host cells to produce RNA polymerase, which transcribes the RNA to create a complementary strand, forming a double helix with both stands. After this the cell will begin to integrate the RNA double strand as its’ own DNA within the nucleus.
A lot of viruses have an envelope, a lipid bilayer that surrounds the protein coat, aiding in the invasion of the host cell by making an easier entry. Many viruses are more complex, containing an additional outer membrane derived from plasma membrane of a cell during exit from the cell.10 After Figure 2, (1) the replication process begins with the attachment to the cellular surface. (2) Once attached the virus will penetrate into the host cell. (3) Within the host cell, the viral DNA is released. (4) Since viruses do not have the capacity for protein synthesis or an energy source, new protein coats are synthesized in the host cell with the help of mRNA. (5) While the capsids are forming, DNA is waiting to combine with the new capsids. (6) Next is assembly in which both parts meet again and the capsids surround the viral DNA, making a complete replication. (7) Lastly, the host cell erupts, releasing the mature viruses to repeat this process in additional cells.
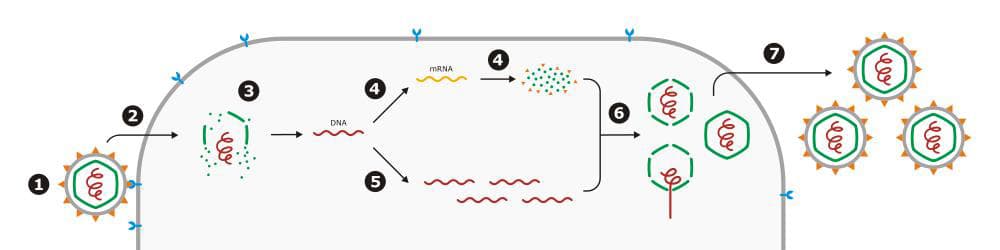
Figure 2 The viral replication process. Courtesy: Drawing of "Virus replication" Wikimedia Commons (public domain)
There are four main strands of the common cold, the Rhinovirus, originating from a virus: 1) the rhinovirus which is the most common and has 99+ variations; 2) human parainfluenza virus; 3) respiratory syncytial virus; and 4) human metapneumovirus.11 The rhinovirus itself can be classified into three species. The determination between species results in the virus’ variance in capsid properties, genome organization, and primary sequencing conservation.12 The cell receptor has just been identified for the rhinovirus C (RV-C) species, which can cause more severe illness than members of the RV-A or RV-B species.13
Immune System
Benjamin Franklin was onto how the common cold can be transmitted from person to person, close quarters and engagement with one another. It is believed that catching a cold is done so through close and personal contact. In general, 80% of infectious diseases are spread by touch.14 Think about that…From shaking hands with someone with a cold or using the same doorknob as someone with the flu or when you watch a student get a drink of water and it looks like they are kissing the water fountain where microbes probably thrive. Catching it is not the hard part, preventing and “treating” it is. When the body encounters a bacterial or viral infection, the immune system goes to work, which includes tissues, organ systems, and specialized defense cells. There are three major defenses of the immune system: innate defenses, adaptive defenses, and the cell-mediated response. “Many of the symptoms that make a person suffer during an infection—fever, malaise, headache, rash—result from the activities of the immune system trying to eliminate the infection from the body.”15 Which raises the question; is it then too late to treat?
W. Mark Saltzman describes the immune system as a defense department for a small country. 16 I will discuss it as if it were a royal medieval castle. I will use structures and functions of a castle in comparison to the structures and functions of the immune system. Picture a medieval castle, the ramparts or castle walls are like the body’s skin. They act as a barrier of defense against the enemy, a pathogen. The castle’s keep, where the Lord of the castle rules from could be compared the primary lymphoid organs (bone marrow and thalamus), the command center of the immune system. Naturally, the castle tower and lookout points could be considered as the informants of immune system, secondary lymphoid organs (lymph nodes and spleen). The different levels of the royal army would be similar to the all the specialized cells (macrophages, natural killer cells, neutrophils, B cells, dendritic cells, and T cells).17
When pathogens enter our bodies, gracing us with their presence there are two parts of the immune system that may be triggered, the innate and/or adaptive responses. The innate response is the defense that reacts immediately and acts within hours, similar to the soldiers of the royal army. It also can recognize different classes of microorganisms or the enemy.18 “The innate immunity is not always completely effective in keeping pathogens out of the body. Some pathogens have developed ways to avoid detection by the innate immune system. In addition, the innate immune system might simply fail to work effectively enough to clear the pathogen before an infection is established.”19
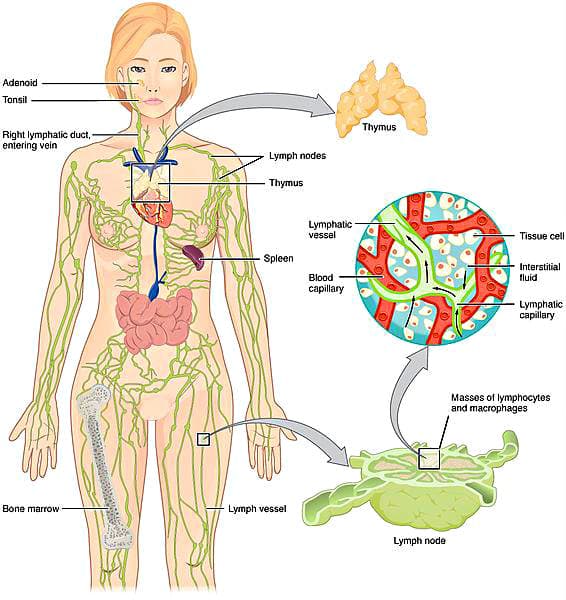
Figure 3 The cellular and tissue structures of the immune and lymphatic systems. Courtesy: Diagram of "Anatomy of the Lymphatic System" Wikimedia Commons (public domain)
If the pathogen is a beast of an enemy, your body will, unknowingly, recruit the adaptive defenses. The adaptive response, which could also be referred to as the commanding officers of the royal army in our prior analogy, may not go to defending against the pathogens for days, and has a more specific recognition of microorganisms. This response is capable of keeping a record of microorganisms it has encountered, acting on the recall when it recognizes it and responds to that pathogen with a specific response.20 Specific cells that work within the adaptive response are B cells and T cells. B cells originate from bone marrow and attack outside the cell’s body, while T cells grow in the thymus and attack within the cell. B cells operate out of the antibody-mediated immunity and T cells operate from the cell-mediated immunity. “Both B cells and T cells are capable of uniquely recognizing specific pathogens.”21
Macrophages operate in both the innate and adaptive responses. This is the most significant cell that surveys the host for viral infections. It has the capability to cause a response when imitated with similar parts of a viruses such as viral RNA. In order to produce cytokines, the macrophage’s surface contains turnstile-like receptor that must interact with the parts of a viral or bacterial pathogen. The cytokines operate to engage other immune cells, provoke inflammation, and create systemic symptoms such as fever.22 These processes or symptoms stimulate immune cells to take action, hinder pathogen growth, and prepare damaged tissues for repair. Macrophages engulf pathogens through the process of phagocytosis. Through this process of phagocytosis, the macrophages’ flexible structure is able to reach the pathogens, like Stretch Armstrong, and break it down by engulfing and eating it.
Lymphatic System
The lymphatic system is tied to many other systems in the body, and it will be discussed in its’ relationship to the immune responses. It produces and distributes cells, lymphocytes and macrophages (members of the royal army), to battle diseases. Within this system, lymph vessels are tasked with draining the fluid from all parts of the body and returning it to the heart. The spleen is a fragile organ that carries the responsibility of filtering blood for pathogens, debris, or weary cells. It is filled with lymphocytes and macrophages that can mount an immune response readily if antigens are sensed. Lymph nodes are found forming along lymph vessels. As lymph passes from a vessel to a node, it begins to doddle and trickle through passageways that are lined with millions of lymphocytes and macrophages. When the lymph node is annoyed and irritated by a pathogen, it will swell.
Antibodies, also known as immunoglobulins, are specialized protein molecules that are generated by white blood cells. These molecules play a vital role in the immune response by distinguishing and binding to specific antigens or pathogens, such as viruses or bacteria, aiding in their demise prior to their entry to cells.23There are five different classes of immunoglobulins: in regards to the rhinovirus I will discuss one, Immunoglobulin A (IgA). IgA is found predominantly in mucus, saliva, sweat, tears and secretions of the gastrointestinal tract. Thinking about where IgA is most found, it makes sense that it works against the common cold because of the symptoms we experience; runny or stuffy nose, mild or sometimes hacking cough, and sore throats, are found in structures that contain a mucus layer for protection. When we catch a cold, it’s no wonder why IgA is our prime antibody working to have our backs.
Biomedical Engineering of Vaccines
The common cold is unlike any other human disease because of two factors: firstly, it is arguably the most common human disease and, secondly, it is one of the most complex diseases because of the number of viruses that cause the familiar symptoms. These two factors have made a ‘cure’ for the common cold one of the most difficult scientific and clinical endeavors. There is a substantial economic impact of common cold because of the large number of consultations to general medical practice. Therefore, there is need to improve the current standards of treatment for the common cold.24 This makes me wonder; how are influenza vaccines developed to have multiple strains in it, while engineers are crossing their fingers and hoping one will be a main strain that can be combated by the vaccine, while the rhinovirus has the opposite issue of many possible strains but a vaccine has not been developed even for one strain?
“Vaccines can be produced to treat infectious disease that are caused by viruses, bacteria, parasites, and other infectious agents.”25 Vaccines are preventative measures against infectious diseases to prolong life through an acquired immunity. They have been proven to be safe and successful for people of all ages around the world, any in many cases they have saved lives. Due to their effectiveness, some infectious diseases that are fatal, like smallpox, have been eradicated or eliminated. There are variables that affect the effectiveness, such as, the disease itself, the strain of vaccine, if there is a specific schedule to follow, the need of boosters over time, age and ethnicity. Vaccines have helped to control against outbreaks of infectious diseases like influenza and the measles. Customarily, vaccines contain a very diluted form of the virus or microbe, resembling the original form. Once administered, it allows the immune system to identify it as an invader to attack and demolish it. This allows for T cells to remember this invader to be later identified in the future and act upon it in the same way, if caught again.
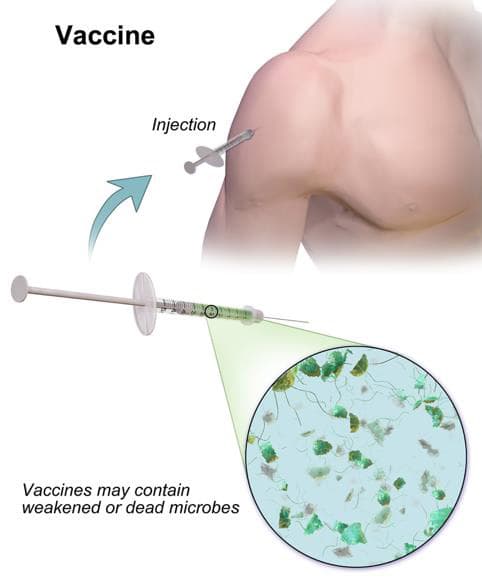
Figure 4 The administration of a vaccine through injection. Courtesy: Diagram of “Vaccine” Wikimedia Commons (public domain)
There are eight different types of vaccines. For the comparison of the rhinovirus and influenza virus, I will discuss the two types of influenza vaccines. The first type is generally known as a killed, inactivated vaccine, which contains particles of the virus grown in a lab and killed. These tend to produce less than robust responses by the immune system. The second type is known as a live, attenuated, vaccine which contain active and spry viruses that have been developed to tone down their toxic effects but are very close to their original state just less menacing. Through this, the immune system is able to trigger a diverse immune response that also provides a more long-lasting immunity. Most commonly, vaccines can be administered through injection or orally, as seen in Figure 4. Side effects can be experienced which include, muscle aches, pain near the injection site and in some cases a fever. When born your vaccination journey begins, continuing with traveling and schooling mandates, this may pose some controversy which will be later addressed.
Human rhinoviruses are considered harmless when compared to more deadly infectious diseases, usually remaining confined to the upper respiratory tract and only occasionally spreading to the lungs. Between the US and the European Union there have been thirteen vaccine trials and three antiviral drug trials for the Rhinovirus. As for the other strains of the common cold there have been an additional seventy-three vaccine trials and fifty-seven antiviral drug trials. Vaccines have proven to eradicate Smallpox and the Poliovirus. However, because of the variations and changeability of the rhinovirus makes it next to impossible to eradicate the common cold.26 When mapping the genome of the rhinovirus there is “ a large degree of sequencing diversity among the rhinovirus manifests as amino acid changes in capsid surfaces.” [rhino book] I can infer that due to the changes or mutations in the just the capsid alone can cause for thousands of different combinations, resulting in an excessive amount of varied genotypes, genetic code, of the rhinovirus. Although it is possible to measure and define relative relationships among any set of existing causes for variations, it is virtually impossible to retrace the exact lineages that gave rise to them.27
Currently across the world, pharmaceutical interventions are being deemed necessary by World Health Organization’s (WHO) Battle against Respiratory Viruses initiative. The RNA respiratory viruses (NIRVs) are responsible for a higher annual morbidity and mortality than influenza viruses, across all age groups. The initiative has highlighted the need for an enhanced clinical and epidemiological surveillance for respiratory viruses.28 When you read how to feel better from the common cold on the Center for Disease Control and Prevention’s (CDC) website the very first statement is, “there is no cure for the common cold.”29 However, they direct you to do drink plenty of fluids and get rest. It may be safe to say that the common cold will always be living among us and we need to better care for ourselves to prevent catching it. This leads me to believe that maybe the best way to inadvertently cure the cold, is to look into our health habits.
Ethical Issues and Vaccines
Vaccines have made quite the impact on the world over the course of decades, from eradicating smallpox to minimizing the serious infections like the measles or polio. There are many debates in regards to vaccinations, such as development, regulation and applications. Here I will discuss issues mainly connecting to the regulation and mandates for our schools, governed by our states. “The first school vaccination requirements were enacted in the 1850s to prevent smallpox. Federal and state efforts to eradicate measles in the 1960s and 1970s motivated many modern mandates policies. By the 1990s, all 50 states required students to receive certain immunizations.”30
Conflicts with vaccination mandates can stem from individuals or communities who appose the mandates due to religious or philosophical beliefs, leading to ethical controversy. For example, the human papillomavirus (HPV), which is a sexually transmitted disease, is currently suggesting three doses of the vaccine for girls, beginning at age 11-12. Naturally, this vaccine identifies the possibility of premarital sexual intercourse in young girls, conflicting with religious and person beliefs of abstinence. Initially, it also raised questions if it is equitable to vaccinate only one gender, why only females? Currently in the United States, it is suggested for all developing children to receive the HPV vaccine.
When there is conflict usually comes some form of negotiation. In the case of vaccination mandates vs. religious or personal beliefs for students within schools, there are now exemptions for students and their families. The entire United States (US) allow such exemptions for medical reasons; addressing personal beliefs and differing vaccination concerns, 96% of the US allow religious exemptions; and 40% of the US provide exemptions for philosophical beliefs. 31 As with any ethical issue, this one is no different in the balancing act of respecting personal beliefs and the best interest for the community, in this case, it is our health. However, with vaccines, it must be all or none.
Conclusion
Throughout the curriculum unit I reviewed what the common cold is and when it is believed to have originated. I first discussed the rhinovirus’ affect on the human body from the cellular to systematic levels. While also discussing the body’s response to defend against respiratory infections. I specifically focused on the respiratory, immune, and lymphatic systems, discussing their functions and relationships to each other. When reviewing the immune system, I refer to the many components similar to a castle’s defense. I also dig into the operations of the innate and adaptive responses all the way down to a cellular level. Later in the unit, I talk about how viruses are structured, also the replication process viruses perform within human cells as hosts. Lastly, after the discussion of viruses, I focus on immunoglobulins and their relevance to protect our bodies. I wrap up with the understanding of why there is not a vaccine for the rhinovirus. Due to some controversy in public education, I tap into the ethical issues of the regulations and mandates of vaccines.
This research and curriculum development is extremely valuable to the work I do inside my classroom. More often than not, as public school teachers, we have to flexible and sometimes “learn as we go.” In some cases, that is the best we can do based on time and additional variables, yet its not deserving of the students I serve. This work has taken the learn as we go mentality and developed my understanding to be specific and thorough. It has allowed me to build a content rich wealth of knowledge before teaching, permitting me to focus on my students’ understanding, not my own.
The common cold is one of the leading reasons why students miss my class and the rest of their school day, resulting in 22 million school days lost annually across the United States.32 With all the variables my students face, they cannot afford to miss school because of a cold. I hope that we can find a cure or develop a vaccine for the rhinovirus. Who knows, maybe it will be one of my students or yours.

Comments: