Background
Structure
Liver cells (also called hepatocytes) are arranged in hexagonal units, an arrangement that allows them to fit together tightly, yet still have contact with three parts of the circulatory system and the bile duct (figure 1). In the center of each hexagonal unit is a branch of the hepatic vein, which goes back to the heart. At each of the six corners of the hexagon is a bundle of three tubules. One is a branch of the hepatic artery, bringing nutrients, oxygen and other chemicals needed by the hepatic cells. The second tubule is a branch of the portal vein, carrying nutrients and drugs directly from the digestive system to the liver cells. The third is a branch of the bile duct. Cells are arranged in a hexagonal fashion, with the central or hepatic venule centralized in each hexagonal unit. Triad bundles are found at each hexagonal corner. In the bundles are a hepatic arteriole, a portal venule and a branch of the bile duct(see figure 1). Bile is produced by the liver and excreted into the bile duct system and is important in fat metabolism. It makes fat soluble, so it can be transported as a fluid. Bile can be stored in the gall bladder, prior to its elimination through the digestive system. The bile system provides a pathway that is often used to eliminate drugs or the breakdown products of drugs, which can also be fat soluble, from the liver. A chemical can be absorbed by the hepatocytes and excreted directly into branches of the bile duct. From there, it can be excreted into the intestines and eliminated from the body. Another way the liver detoxifies chemicals is by converting them into metabolites, which are more easily excreted by the kidneys or intestines.
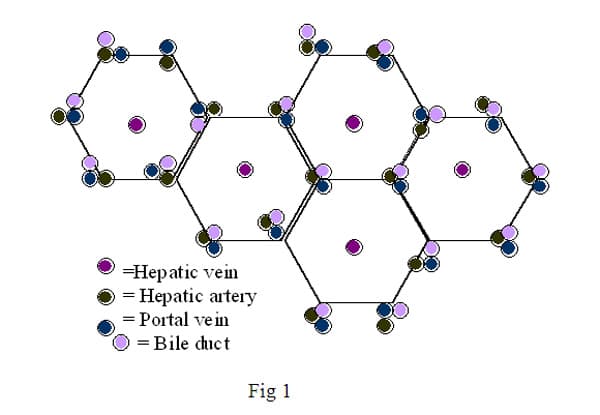
The bundle of three tubules at each corner of the hexagonal hepatocytes plus the central hepatic vein constitute the functional parts of the blood and bile circulation, which are intimately connected to the liver. In general, the circulatory system is straightforward. Blood goes from the heart to the lungs with a high percentage of carbon dioxide and comes back to the heart with a high percentage of oxygen. It then goes out to the various organs with oxygen and comes back to the heart with more carbon dioxide again. Circulation through the systemic and pulmonary vessels can be compared to a figure eight with the heart at the intersection. The liver adds some complexity to that system. It receives oxygenated blood from the heart through the hepatic artery. It also receives deoxygenated blood from the intestines through the portal vein. This blood is rich in nutrients and toxins and goes through the liver before going to the rest of the body. The liver is the only organ that receives multiple circulatory systems, which is a measure of its importance.
Functions
The liver works as a blood filter. It contains a high proportion of phagocytic cells, (Kuppfer cells). These are macrophages, a type of white blood cell, which go into and out of the circulatory system. Most of them are found in tissues, prowling for foreign objects to destroy. It is estimated that most of the fixed macrophages in the body are the Kuppfer cells in the liver. Because so much of the blood supply is shunted through the liver, the Kuppfer cells have the opportunity to phagocytize many foreign particles. For example, Kuppfer cells in the liver routinely scavenge old red blood cells, the main solid component of blood and our transport mechanism for oxygen. The actual transport protein for oxygen is hemoglobin, which contains iron. As the liver breaks down the red blood cells, the proteins are also digested for reuse of the components. To do this safely, the iron molecules that are released then have to be stored for reuse in a non-toxic form. The iron is generally coupled with ferritin to protect the cells in the liver from toxic effects of iron. Kuppfer cells can also phagocytize bacteria, small parasites, and circulating toxins.
The liver is important in detoxifying poisons. As previously mentioned, the toxins can be exported from the liver to the intestines through the bile duct. Usually, toxins are metabolized to a more soluble form. Sometimes they are metabolized by the hepatocytes and then sent into the venous circulation, where they are filtered by the kidneys for excretion. Urea is made by the liver and travels to the kidneys for concentration and excretion. Urea is especially high in nitrogen, a component of amino acids, which the liver cells digest. Liver cells package the excess nitrogen into urea, which can be excreted.
One of the toxins produced by breakdown of the hemoglobin, the oxygen carrying protein in red blood cells, is bilirubin. Macrophages phagocytize old red blood cells, breaking down the hemoglobin and releasing free bilirubin into the blood that is then bound to albumin. Hepatocytes take in the bilirubin that is loosely bound to albumin. Within the liver cell, bilirubin is conjugated with glucuronic acid. In this form, it is soluble and can be released into bile. Increased levels of bilirubin cause jaundice. Jaundice is the yellowing of skin and eyes that is an external indicator of major liver damage. The levels of both conjugated and unconjugated bilirubin can be informative of what kind of liver disease a patient has.
The hepatocytes are also involved with breaking down nutrients. They are especially important in the digestion of fats. Hepatocytes make bile, the main function of which is to make fats soluble in blood. The cells of the body can then absorb the fats for nutrition. Bile is also an excretory route for various metabolites of toxins. Bile contains bile salts, bilirubin, cholesterol and other compounds. These compounds can be concentrated and stored in the gall bladder. Bile helps maintain body cholesterol levels through control of its excretion rate. It is part of the mechanism for excreting heavy metals. Many of the contents of bile secreted by cells are reabsorbed and recycled to the liver and gallbladder.
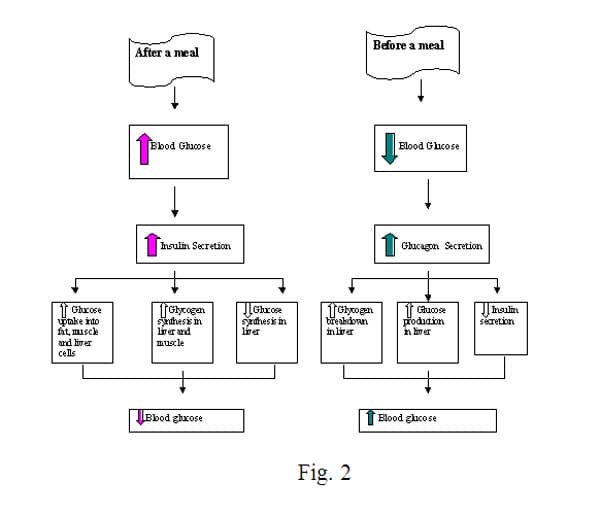
One of the most important roles of the hepatocytes is to aid in the control of the blood sugar. We always think of the pancreas controlling blood sugar through insulin, but, in fact, the liver also plays a major role. The liver stores glycogen, a polymer of glucose molecules, which can be digested for release into the bloodstream when glucose levels are low. Glucose is the simple sugar that cells use for energy. The liver is involved in the feedback system controlling the amount of glucose in the blood. Blood levels must remain relatively constant, because glucose must be kept at a level necessary for proper brain cell function. Once the glucose level goes down too far, the brain cells start dying. Insulin, when secreted by the pancreas, lowers the glucose concentration, but the liver is a major site of action for insulin, and it is the key to not letting blood sugar get too low (figure 2). Hepatocytes are also capable of gluconeogenesis, making glucose by converting amino acids and simple sugars to glucose. Other cells can only break down glycogen (or other complex forms of glucose polymers) into glucose. The liver can actually transform other molecules into glucose.
Figure 2 is a simple flowchart showing the regulation of blood glucose by fat, muscle, and liver cells, which is orchestrated through insulin and glucagon. After a meal, the flow chart on the left shows that the blood glucose goes up, causing increased insulin secretion by the pancreas. Insulin acts on fat, muscle and liver cells to take up more glucose. Glycogen synthesis from glucose is increased in the liver and muscle cells and glucose synthesis via gluconeogenesis in decreased in the liver. These actions result in a decrease in blood glucose level. The flow chart on the right shows the opposing actions during low blood sugar, as in before a meal. Low blood glucose increases glucagon secretion by the pancreas, targeting the liver. In the liver, this causes increased glycogen breakdown into glucose and also increased gluconeogenesis. The pancreas decreases insulin secretion, all acting together to increase blood glucose.
The liver is also important in the production of cholesterol, a fat that all of the cells in the body need. Cholesterol is absolutely essential for the healthy function of cell membranes; it is also the starting chemical for the synthesis of steroids and vitamin D. It is important in protecting the skin from water or evaporation, and forms the sheath around nerve cells, which aids in the signal going all the way to the end of the axon, especially very long ones. It is not broken down for energy. As was previously mentioned, excess cholesterol is excreted in bile. When we talk about "good" cholesterol vs. "bad" cholesterol, in general, the liver makes much of the good cholesterol and much of the bad cholesterol is from food sources, specifically from animals. It is not found in plants.
Fat-soluble vitamins are metabolized and stored in the liver. As mentioned above, the liver uses cholesterol to make Vitamin D, which has been considered a fat-soluble vitamin for many years. But, biochemists are currently classifying it as a hormone. Vitamin D is also stored in the liver. Vitamin D is necessary for absorption of calcium. Vitamins A, E and K are all metabolized and stored in the liver. All are necessary for the health of humans in various ways. Vitamin A is part of the pathway the eye uses in adapting to low light, i.e. night vision. Vitamin E is an antioxidant, probably preventing oxidation of unsaturated fatty acids. Vitamin K is used in the clotting of blood, along with fibrinogen, a protein made by the liver, coagulation factors, and platelets.
The liver is responsible for several other important jobs. Copper is stored in the liver. Many important proteins are synthesized by the hepatocytes, such as albumin, carriage proteins (that bind and transport hormones and other substances) and coagulation factors, important in blood clotting. Coagulation factors are another way to test for liver function, since if it is not producing coagulation factors, the blood does not clot as quickly.
Tests for liver function
There are several laboratory tests for liver function. Two tests, which are generally ordered together, are blood tests for the enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST). These are not specific tests, but are indicators of liver tissue damage and necrosis. Doctors also look at the ratio between them for further information about the site and extent of the damage in the patient Alkaline phosphatase is also a non-specific enzyme that is elevated in liver disease. Elevated bilirubin can also be tested for and indicates liver disease or sometimes a disease causing increased breakdown of red blood cells. Prothrombin time, a test for coagulation of plasma, can also indicate liver disease or damage resulting in a lack of liver produced coagulation factors. Testing for albumin levels is another test. The protein albumin is made only by hepatocytes and is abundant in plasma, so a low level of albumin or even total protein, can be an indicator of liver damage. There are also tests for the viruses that cause hepatitic disease. The florescent monoclonal antibody tests for hepatitis B antibody (HBAB), hepatitis B core antibody (HBc), and hepatitis B surface antigen (HbsAg) have been available for many years. The test for HCV antibody has been available since the nineteen nineties. These are standard immunology tests for hospital labs and in fact are done on all donor blood before it can be transfused, since HBV and HCV are infectious through blood products.
Factors affecting the liver
Many things can affect viability of hepatocytes. In the documentary, SuperSize Me, which is about the effects of processed food on our bodies, the writer/ director/ central character eats only food from a well known fast food restaurant for thirty days. His doctor finds increased liver enzymes (ALT and AST), which are laboratory indicators of liver damage, within two weeks of starting the diet and diagnoses him with fatty liver disease, which can be a life threatening disease leading to cirrhosis and possible death. Since Morgan Spurlock is healthy at the beginning of the thirty days and does not drink alcohol, the obvious culprit is his diet of processed foods. Although this was not a controlled study, there have been many studies examining the negative effects of processed food and so this anecdotal evidence seems to point towards processed food causing the fatty liver. Fatty liver disease is normally found in women with Type II diabetes, who are obese, and/ or have hyperlipemia (high lipid or fat levels) in the blood. The fact that Mr. Spurlock gained almost twenty pounds in the first two weeks of the diet seems to mimic some of the effects that normally cause non-alcoholic fatty liver disease.
Hepatitis B Virus (HBV) is a DNA virus, that is transmitted by exposure to body fluids. In the USA, it is commonly spread through sexual contact, needle sharing, or mother to child during pregnancy or childbirth. It was a common infection of health care workers until the early to mid-nineteen eighties, when HIV became widespread. At that point universal precautions were put in place and latex gloves and hand washing were required any time there was contact with blood or body fluids. The incidence of new cases of HBV among health care workers dropped dramatically. Severe allergies to latex increased, but that is a different story. An effective vaccine to HBV became available in the early nineteen nineties, soon after universal precautions were required, dropping new infection rates even more.
HBV infection can manifest in three ways. It can be asymptomatic, with the patient not realizing he or she is infected unless tested. It can cause acute liver disease, which usually resolves within six months. And it can become chronic, with the person shedding virus for the rest of his or her life. HBV can be spread during the asymptomatic, but active, disease phase. It is one of the most common sexually transmitted infections (STI's) and protection against spread should be used during sexual activity. The virus targets hepatocytes and causes liver damage, often necrosis (death) of the cells. It can also cause fibrosis, where too many matrix proteins, such as collagen, are produced which replace the liver cells, and eventually cause cirrhosis. Cirrhosis is a build up of scar tissue in the liver, which eventually impedes liver function. The hepatocytes may regenerate, but the intimate contact with blood vessels that is so important for normal liver architecture and function, is lost. When cirrhosis occurs, illness can be caused by the loss of the important substances that the liver produces. The build up of toxins from the bile not being channeled properly can also cause systemic damage. Finally, the role of the liver in glucose regulation can cause great damage to the rest of the body, since the liver plays an essential role in maintaining sufficient glucose in the blood (i.e. brain damage can result from low blood sugar).
Chronic HBV can develop after asymptomatic or acute infection. It can result in long-term damage to the liver. HBV virus in present in the infected person's blood and is constantly shed. The HBV positive person can spread the virus through sexual transmission or blood and may not realize it until there is a reason to screen him or her for hepatitis.
HCV is the virus responsible for most of the viral infections formerly called non-A, non-B hepatitis. It is most commonly spread through shared needles. It is a common infection amongst IV drug abusers. It is also an infection that is frequently spread through tattoos and piercings with a dirty (i.e. reused or improperly sterilized) needle. More than half of people infected with the virus progress to chronic disease. The virus can cause fibrosis and cirrhosis of the liver. It is a more aggressive chronic disease than that caused by HBV. It is the most common reason for liver transplantation. HCV also exacerbates liver damage from other illnesses or drugs.
Many drugs cause liver disease, including acetaminophen, the pain reliever in Tylenol; acetylsalicylic acid, or aspirin; many prescription medications; illegal drugs of abuse; and alcohol abuse. Since OTC drugs are part of the state standards for health and they seem to be misunderstood by almost all of my students, I will focus on acetaminophen.
There is great concern about acetaminophen overdose due to several factors. It is extremely toxic to the liver in high doses. Many people, especially teenagers, consider it safe because it is so freely available. It is added into many OTC and prescription medications, so it is relatively easy to overdose if you are not aware of the ingredients in your medications. OTC cold and flu remedies frequently contain acetaminophen. Often people use the old adage more is better and combine various drugs and/or take them in higher doses than suggested, including taking some Tylenol for their fever. You could potentially take several drugs containing acetaminophen without realizing it, if you do not read the labels carefully. Some people use it for suicide attempts since it is so readily available, as well.
Acetaminophen is considered an intrinsic hepatotoxic drug due to the frequency of damage done to the liver when the drug is used improperly. People with previous liver damage can be affected even at normal dosage. Alcoholics and people with active cases of HBC or HCV are especially susceptible. It is believed that there are many more cases of drug induced liver damage than are reported. It is difficult to diagnose. The damage is exacerbated by other factors, such as previous liver damage by alcoholism and viral hepatitis. It is also much more damaging in obese and anorexic patients.
Acetaminophen affects the mitochondria within the hepatocytes, causing the mitochondrial membrane to become more permeable, which results in disruption of the cytoplasm and loss of much of the ATP of the cell. The mitochondria, which are small organelles inside each cell in the body, are responsible for the energy production and storage for the cell. They use oxygen and nutrients to convert molecules of ADP to ATP, which uses energy to go from two phosphate groups in each molecule to three. When the ATP is converted back to ADP by removing a phosphate group, energy is released for use by the cell. If the cell has no energy available to make protein or facilitate transfer of necessary molecules into the cell or any of the other millions of jobs it needs to do, it will rapidly die.
Some mushrooms can also cause liver failure. The most frequent cause is Amanita phalloides. Generally, the mushroom is eaten accidentally by confusing it with edible mushrooms. It is a good idea not to pick your own mushrooms or eat the ones picked by someone else unless they are known to be an expert. Mushrooms are easily confused. Amanita apparently produces a toxin that inhibits RNA polymerase. RNA is vital to all cells, since it is necessary to protein production.
Liver transplants
Transplantation of livers is relatively new. Currently, HCV infection is the number one indicator for transplant. But there are other indications, including liver damage from alcoholism or HBV infection or many other causes. In general, the build up of scar tissue is an indicator for transplant, since the cells regenerated by the liver are blocked from necessary vascularization by the scar tissue. As we have seen, vascularization is extremely important to hepatocytes and each one must be within diffusion distance of a branch of the hepatic vein, a branch of the portal vein from the intestines, a branch of the hepatic artery and a branch of the bile duct. Without all of these, vital chemicals such as cholesterol cannot be manufactured, glucose regulation cannot be done, toxic substances, such as drugs and bile, cannot be excreted.
Transplants can be obtained from a cadaver liver. In that case, because of the regenerative properties of hepatocytes, the liver can be split in two and given to two recipients. Transplant surgeons have also been doing designated liver transplants to patients, usually from a relative or close friend. Since this is a serious operation on the donor, with a lengthy recovery time, there are many steps and safeguards around the procedure. But a partial liver can regenerate in both the donor and recipient. Obviously, if the recipient has an active case of HCV or HBV, this can easily escalate with a new liver to infect. Doctors treat the patients aggressively with antiviral agents. There is no cure, but the disease can be kept under control better. For alcoholics, it is complicated by their addiction. If they go back to drinking large quantities of alcohol, the transplant becomes a temporary solution.
Transplant ethics
We have all seen the movies and read the books about evil organ dealers putting people into a coma and harvesting their organs to sell to rich people. Sometimes the stories are about immigrants being forced to sell a kidney for protection from deportation. Jodi Picoult wrote a story of a family who deliberately had a second child to provide bone marrow transplants for the first. It examined the issues around whether a person owns their own body. Is it legal for parents to demand that one child give transplants to another? There was a recent governor's decision to free a prisoner if she would donate a kidney. I have a friend with Lupus whose sister donated a kidney. She was happy to do it, but it was a temporary measure and the recovery time for the donor was not easy. How do they decide who gets a transplant, whether it is from a dead donor, as with most transplants, or from a living one, as can be done with livers, kidneys and bone marrow?
Who should donate an organ, specifically a part of the liver? If you have a child dying of liver failure, the impetus to donate could be overwhelming. It seems like a huge commitment from a friend, more distant relative, or a stranger. Liver donation is not a simple thing, it takes time to recover from, it can result in ill health or occasionally even death. Is it ethical to pay someone to donate part of his or her liver for a transplant? Do we want to live in a world where all medical issues are decided by money and big business? It seems like we are headed that way with private insurance companies controlling what procedures are done and not done for those of us without unlimited funds. What about forcing someone to donate? Prisoners have been forced into being experimental subjects in the USA before. Should we value contributing members of society over the non-contributing? (We can analyze our current values system by comparing money spent on schools to money spent on prisons, comparing salaries for working people like plumbers, teachers, waiters, to so-called celebrities, actors, football players, etc.) At what point do we become like Josef Mendel, experimenting without conscience on the mentally and physically disabled, torturing twins to see whether their reactions differ? This may be an exaggerated concern, but it has happened to greater or lesser extent in modern medicine. Even donations from cadavers can be controversial. Some families of donors object strongly to their dead relatives organs being used, even if the donor gave permission when alive. Another controversy would be to harvest organs from brain dead people, keeping them "living" until the organs can be used. Now we keep our dying alive in pain and indignity, would it be worse to do it for a reason besides fear of lawsuits?
In reality in the USA today, most states request drivers to agree to donate organs as an option when they renew their driver's licenses. They are only listed as donors if they take an active step to become one. If their families object to donating organs when the person dies, they override the expressed wishes of the deceased. In our lawsuit happy society, it is deemed better to lose the organs than to take a chance on lawsuits and bad publicity. Organ sales are illegal in the USA, but there is a black market in many countries and wealthy Americans often buy the organs. There have been suggestions that we make selling organs such as kidney, liver and bone marrow legal, with a set price for each organ.
Another difficult problem is deciding who gets the donated organ. Life and death decisions are made since there are never enough organs for the recipients. Physicians have to worry about age and chances of survival. What about whether the recipient deserves one? If an IV drug abuser has HCV, should they get a new liver, having brought on liver disease through their addiction? Would the liver even last? Drug addicts recover so infrequently. Would someone who contracted HCV through getting a tattoo at a party deserve a new liver? Should they be punished for one stupid decision? Should prisoners be placed lower on a list than upstanding citizens? What about someone in prison for marijuana use vs. someone convicted of raping and murdering a child?
In the USA, these issues are mainly decided by doctors who specialize in transplants and by UNOS, a private organization that is contracted by the federal government to maintain all the data on transplants and make the matches based on histological compatibility (so minimizing the chance of organ rejection), the likelihood of success and the probable length of post surgical life. So, a young, healthy person in need of a transplant would be more likely to be high on the list than an older healthy person, if all other factors are equal. Much of the inequity is found at the first level, the transplant doctors who recommend patients to UNOS. Since their highest priority is getting paid, the wealthy and people with the best medical insurance are likely to be highest on their list of recommendations. Surprisingly, at least to me, prisoners have ready access to transplants, being among the few Americans with free comprehensive health care.
Artificial livers
Replacing a failing organ with an artificial one has been successful in a limited way for many years. Dialysis for kidney patients has been available and has been refined to a simple and effective system. There is a similar system now available to those with liver failure. Blood is removed from the body and returned in a similar manner to dialysis. In this case, blood cells are strained out, separated from the plasma and returned to the body in plasmapheresis, the first step. Plasma is then physically filtered through charcoal to remove relatively large foreign objects. Plasma is then pumped through a hollow-fiber bioreactor, in contact through a membrane with cells outside of it. Pig liver cells are used, since the hepatocytes function similarly to human hepatocytes. Since there is no actual physical contact between the human cells and the pig liver cells, there is no immune reaction. The liver cells are then stimulated to produce the many hormones, proteins, bile, albumin, and other chemicals by the low concentration of them in the plasma. It is not perfect. Next to the natural organs, with their constant monitoring of levels of necessary nutrients, toxins, etc., this is an inefficient system. But, it can keep a patient healthy and with a reasonable quality of life while on a list for a liver transplant.
What about the dream of an artificial liver that goes into the body to replace the old one and settles in and does its job for years? It may happen some day. Liver cells can regenerate. They do not do well in cell culture, but we may find new techniques to overcome that. Some day, we may be able to vascularize a structure in the same elegant manner as the liver. If the vessels and ducts are not bringing sufficient blood, or taking away sufficient waste, no cell replacement will work. Each hepatocyte has its own network so that it can take in all of the things mentioned and take away all of the things mentioned and more. They do not specialize, so they must all be in contact with vessels and ducts.
Endnote
As the money becomes scarcer, people live longer with more illnesses and insurance companies bring in record profits, some tough decisions lie ahead about even pursuing these goals. Can we afford to keep the rich alive longer and longer, but refuse to provide the most basic medical care to the rest of us? We currently have the highest child mortality rate in the developed world. It is a brave new world, but how can all of us enjoy its fruits?

Comments: