Background Content
Air Pollution
Air pollution affects the air we breathe outside our homes, but also affects our lives indoors. This unit will highlight respiratory illnesses that arise at home and at the workplace. Though there are many pulmonary diseases including lung cancer, this unit will cover chronic obstructive pulmonary disease through asthma, restrictive pulmonary disease through silicosis and second-sand smoke from electronic cigarette exposure. It is my intention for students to study a mixture of respiratory ailments that have a long history and those that have recently developed. This broad exposure will introduce them to many concepts in respiratory physiology, and improve their understanding of respiratory health.
The Environmental Protection Agency (EPA) is charged with assessing air quality. The EPA has identified six pollutants in the air as being the most critical and therefore requiring the most attention. They are carbon monoxide, lead, nitrogen oxides, ozone, and particulate matter. Particulate matter varies in size, shape, and source. The Center for Disease Control (CDC) classifies them as being of two major groups: primary and secondary. Primary being the source of the particulate matter and secondary being those that react with sunlight and water to create particles. For example, road dust is a primary source and exhaust from cars is a secondary source. When studying air quality, particles of 2.5 micrometers are measured, since at this size, dust can become trapped in the furthest parts of the lung, the alveoli. There are different types of particular matter, organic and inorganic. Particles like grain, cotton, and animal dander are considered organic because they contain carbon, whereas metals, soil, clay, are inorganic.14
According to the EPA many areas of California, including the Sacramento, Central Valley, and San Joaquin Valley violate national ozone and particulate standards. The city of Los Angeles gets the dubious distinction of having the most polluted air among larger cities that include New York, Chicago, and Houston. In fact, one neighborhood, Huntington Park which has a 95% Latino population, became known as “Asthma Town” for its high amount of children with asthma.15 The reason for the poor air quality in these cities include emissions from industrial sources (factories, refineries, mining, and materials-processing plants), transportation, and power plants.16 If air pollution were controlled or managed, a 10% reduction of PM2.5 would save 400 people in Los Angeles, and 1,500 in California, and 13,000 across the nation.17
Since 2014, all of California is categorized as experiencing severe drought conditions, and 70% of the state is categorized as “extreme” or “exceptional” drought conditions. The bread basket of California, once known for its rich agriculture valleys, are turning into the new Dust Bowl.18 California’s ever increasing drought has changed the once fertile valleys into cracked, dry, and dusty lands. Those left to farm, cultivate, and harvest are exposed to higher levels of particulate matter and dust in the air. Thus, it is understandable that air quality in California will become worse and will lead to further increases in respiratory ailments
Beyond the United States, situations are even worse. In countries like India, parts of Africa, and China smoke from the burning of trash, industrial and vehicular emissions, and coal-fired emissions have clouded the sky and the sun so thick that lung disease, eye disease, and vitamin D deficiency is common place. The similarities of countries with poor air quality include high numbers of people who are impoverished, smoke, obese, diabetic, uninsured, and live in high population density areas.
Anatomy and Physiology of the Respiratory System
There are two types of respiration that occurs in the human body, external respiration and internal respiration. External respiration involved the nasal passages, pharynx, and larynx, trachea, bronchi, and bronchioles, and alveolus. This set of tissues provides for the exchange of oxygen and carbon dioxide between air and blood. Cells within tissues all over the body use oxygen to fuel cellular internal respiration, which leads to carbon dioxide accumulation. Internal respiration is the exchange of gases between the blood and cell’s, either to fuel cells with oxygen or to remove carbon dioxide. 19 This exchange of gases between the body and the external world is the job of the lungs.
The lungs are actually comprised of five lobes (two lobes on the left and three lobes on the right). The five lung lobes and their air passages (trachea, bronchi, and bronchioles) are housed in the thoracic cavity. All the major organs of external respiration lie in this space, including the heart, which is necessary to pump blood which transports the gases from the lungs to the rest of the body. The lungs are surrounded by two membranes, the parietal and visceral pleura. The process of breathing, discussed later, involves a large thin muscle below the lung known as the diaphragm, which separates the thoracic cavity from the abdominal cavity.
The upper respiratory tract includes the structures of the nose, nasal cavity, paranasal sinuses, and pharynx. The first structure of contact between outside air and the human body is the nose and its opening – the nostrils. The nose is divided into two chambers by the nasal septum. As air enters the nose it passes through the nasal conchae, shell like structures that line the nasal cavity. The nasal cavity is more than just a simple passage. This cavity and the nasal conchae increase the surface area for olfactory receptors (smell receptors), hair, blood vessels, and mucous membranes lining the nasal cavity. There, epithelial tissues, (cells lining the cavity) and its goblet cells coat the nose with mucous to create a sticky surface for debris. Similarly, hair creates a tangled web that can trap dust before entering the upper throat, the pharynx. Blood vessels warm the passing air to body temperature and the olfactory receptors stimulate the brain to create the sensation of smell. 20
The throat or pharynx is divided into three sections: the nasopharynx, oropharynx, and laryngopharynx. The pharynx leads to the voice box, or larynx. Here, the two sets of vocal cords are housed in cartilage which shape the way sound is produced. Relaxed vocal cords expose the glottis, the hole through which air passes to the main trunk of the respiratory system, the trachea. When food or liquids enter the throat, the epiglottis covers the glottis to prevent food or liquid from entering the trachea preventing choking.
The trachea and lung tissue is analogous to an upside down tree with multiple branches called bronchi. The main trunk, the trachea, is comprised of a series of 20 cartilaginous “C” shaped rings which prevents the air passage from collapsing. Soft tissues between the C-rings allow the trachea to expand. Two main bronchi, right and left, branch off the trachea. These primary bronchi lead to a smaller passages known as bronchioles, which lead to even smaller passages until the bronchioles become alveolar ducts. At the end of each tiny alveolar duct is an air bag, the alveolar sac.21
Each alveolar sac is analogous to a grape bundle with many microscopic alveoli. The alveolus is roughly ~ 300 µm in diameter. 22 It is estimated that the human lung contains about 300 million alveoli. Each single cell lined alveolus is wrapped in capillaries, blood vessels that allow oxygen and carbon dioxide to be exchanged. Because of the thin nature of the alveolus and it being the terminal end of bronchial tree, particles from dust, nicotine, and other air pollutants can easily damage the alveoli. The damage can lead to the equivalent of scar tissue, preventing the fragile alveoli from being able to exchange gases with the surrounding blood vessels.
Breathing
As mentioned previously the lungs are surrounded by a membrane, called the pleura. The pleura is actually two layers, one attached to the thoracic wall, the parietal pleura and the other attached to the lung tissue itself, the visceral pleura. Between the two is the intra-pleural space. The process of breathing includes two major processes: inspiration and expiration. In order to understand the mechanism students need to under two basic rules. One, gases move from an area of high concentration to an area of low concentration. Second, according to Boyle’s Law, pressure is inversely proportional to volume. Therefore, for a fixed number of molecules at a fixed temperature, any pressure increase corresponds to a decrease in volume. The equation P1V1 = P2V2 describes Boyle’s law which can be applied to mechanism of breathing.
To understand how the lungs work students should know the different pressures governing the thoracic cavity. The atmospheric pressure (Patm), the pressure outside of the lungs, is typically 760 mmHg. The alveolar pressure (Palv), the pressure inside the alveoli is also 760 mm Hg if there is no air flow. Intrapulmonary pressure (Pip), the pressure of in the pleural space is about 756 mm Hg. Finally, transpulmonary pressure is difference between the intrapulmonary pressure and alveolar pressure, about -4 mm Hg. This difference in pressure allows the lungs to remain inflated.
During expiration and inspiration the alveolar pressure and the intrapleural pressure change. For example, during inspiration the lung expands: the alveolar pressure drops as alveolar volumes increases. This drop of pressure in the lung creates a gradient (lower pressure in the alveoli compared to outside air), and causes gas molecules to move from the atmosphere into the lungs. Lung volume expansion is created by muscles: the diaphragm drops, the intercostal muscles contract, and the chest rises. The opposite events occur during expiration, decreasing lung volume and increasing pressure: a gradient of pressure is created (higher pressure in the alveoli compared to the outside air). Responding to this gradient, gas molecules from the lungs, including CO2, move out into the atmosphere. This movement is created by the rising of the diaphragm and the relaxation of the intercostal muscles, which decrease lung volume. It is important to note that normal expiration is passive process. The relaxation of the intercostal muscles and diaphragm aid to decrease lung volume.
Essentially, breathing is the movement of gases from a region of high pressure to low pressure. The flow of oxygen into the alveolus is affected by the resistance in the respiratory passages like the bronchi and bronchioles. The flow of air is linear with respect to pressure drop as depicted in the equation:
(Equation 1) ∆P=VR, 23
where ΔP is the change in pressure or pressure difference (gradient of pressure), V is the volumetric flow rate of gas, and R is the resistance to flow.
If resistance in the bronchi were to increase, i.e. constriction of the bronchi, then flow would decrease. Alternate, the pressure gradient required to maintain a flowrate increases as the resistance to flow increases. Other factors also affect alveoli’s ability to expand – lung compliance. The ability of the alveoli to change its volume as trans-pulmonary pressure changes describes lung compliance. A decrease in lung compliance, means there must be a greater change in pressure to increase volume. Another factor that influences ventilation of the lungs is elasticity, which is the ability of the alveolar tissue to recoil after being distended. This is affected by surface tension, which resists distension of the alveolus. Essentially, surface tension acts to pull or collapse the alveolus. This force is mitigated by the presence of surfactant which coats the alveoli. Surfactant has both hydrophobic and hydrophilic groups which binds to the water molecules on the surface of the lungs and thus reducing surface tension. The presence of surfactant reduces the amount of pressure the alveoli must overcome to inflate.
At the alveolus, partial pressure of oxygen dictate the movement of the oxygen and carbon dioxide into and out of the alveolus and capillaries (site of gas exchange in the cardiovascular system). Partial pressure of oxygen is the pressure exerted by oxygen (O2) in a mixture of gases which includes nitrogen (N2), carbon dioxide (CO2), and other gases. The changes in concentration of these gases dictate the movement of gases between the alveolus and capillary membrane. When inspiration, or the movement of fresh air into the lung, increases the partial pressure of oxygen within the alveoli, it is equivalent to increasing the concentration of oxygen molecules inside the alveolus. Through the process of diffusion, O2 moves from the alveolar gas phase into the blood within the capillaries, where oxygen concentrations are lower. During expiration, the CO2 levels from pulmonary arteries move CO2 into the alveolus to be expelled.24 This cycle of exchange is important to understand as it is the mechanism that becomes altered in states of diseases and respiratory distress.
Lung Capacity and Lung Volumes
The amount of gases inside our lungs can be measured using a spirometer, see Figure 1 Lung Capacity. Using this simple machine, lung volumes and capacities can be measured. Total lung capacity (TLC) is the maximum volume of the lungs after maximum inspiration. This volume differs between females and males, with males having a higher TLC. Male TLC is about 6 liters and female TLC is close to 4.2 liters. Vital capacity (VC) is the amount that can be exhaled after maximum inspiration. Residual volume (RV) is the amount of gas left in the lung after max expiration. RV represents about 20% of the TLC. The combination of VC and RV is the TLC. The rise and fall of the lung volume during normal inspiration and expiration is the tidal volume (TV). This volume ranges between 7% to 8% of the TLC. Inspiratory reserve volume is the amount of air subtracted from the TLC and the TV. Expiratory reserve volume is amount of air available beyond the tidal volume. Functional Residual Capacity is combined volume of the expiratory reserve volume and the residual volume. The vital capacity is the maximum amount of air that can be expired after maximum inhalation.25 It is important to understand lung capacities and volumes to understand how disease affects our normal gas volume levels.
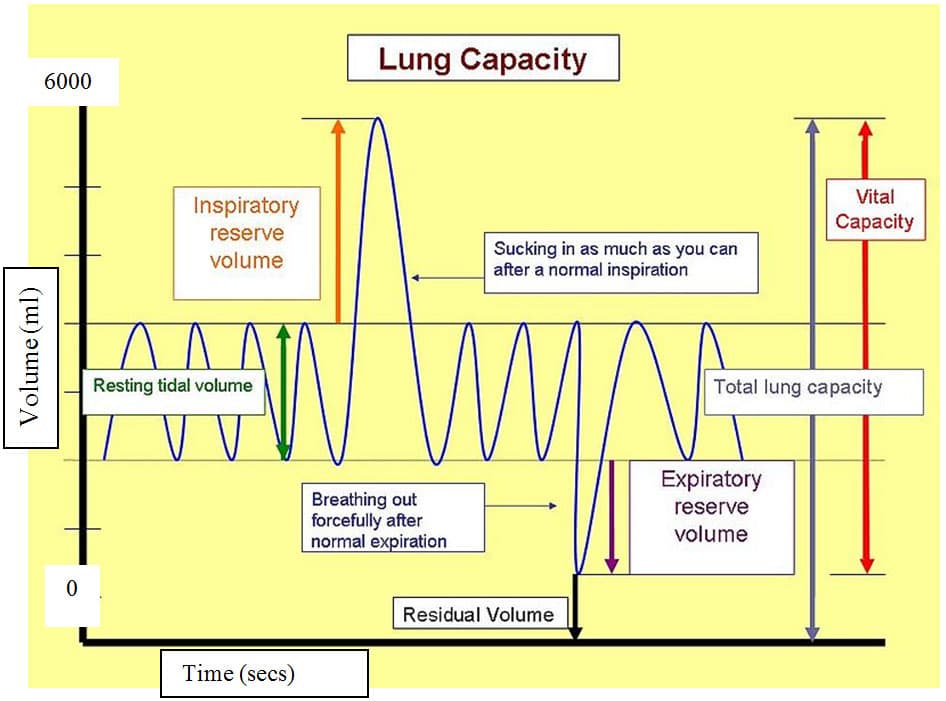
Fig 1: Lung Capacity. 26
Air Pollution and Obstructive Respiratory Disease
We like to think of our homes as sanctuaries. Inside the confines of our four walls and roof and we build a place of domestic bliss where the hearth warms not only our bodies but fuels it from the food we prepare. In first world countries, this is achieved in safe conditions and we think very little of ill effects of cooking a meal for our families. However, in many other countries, this simple act of cooking can be deleterious to our health and to all those whom we live with.
As of March of 2014, it is estimated that 3 billion people cook over open indoor fires, using solid fuels like wood, animal dung, crop waste, and coal. This daily practice contributes to over 4 million deaths from accidents, COPD (Chronic Obstructive Pulmonary Disease), and lung cancer. Moreover, COPD accounts for 22% of the 4.3 million people who die prematurely from illnesses attributed to household air pollution.27 Those who cook over open fires are usually in homes that are poorly ventilated and often expose young children to PM particles 100 times higher than what is considered safe. The effects to one's respiratory health include higher chances for developing childhood pneumonia, COPD, and lung cancer.
COPD is the fourth leading cause of disease and death in the United States.28 Because of its prevalence, COPD, which includes asthma, emphysema, and chronic bronchitis, should be focus in a study about respiratory health. Emphysema and chronic bronchitis are diseases that affect the bronchioles and alveolus. For the purpose of this unit asthma will be the focus since it is a familiar disease to many of my students. Besides inhalation of dust, soot, and smoke, a National Resource Defense Council (NRDC) study of Latinos in Southern California and Mexico border have found that living near freeways and heavy traffic areas increase the number of children with asthma. An interesting fact my students can relate to is that two million Latinos in the US suffer from asthma. NRDC’s study concluded that busy urban cities are hot spots for asthma. These include Boston, the South Bronx of New York City, and Chicago.29
Asthma is a chronic disorder of the conducting airways, in which bronchoconstriction occurs due to increased sensitivity to various stimuli inciting an allergic attack. Asthma symptoms includes inflammation of bronchial walls and production of mucus.30 There are two major types of asthma, atopic and non-atopic. Atopic asthma is the most common type of asthma, called type I hypersensitivity. In atopic asthma immune cells become activated usually preceding an already pre-existing condition like rhinitis (inflammation of the mucus membrane) or eczema. In non-atopic asthma, people experience asthmatic episodes due to other triggers like air pollutants and irritants.31 In large cities pollutants and irritants from exhaust, manufacturing, stress, and everyday chemical irritants can trigger an asthma attack. In low-income countries where cooking is done through an open fire, small particles from the burning of wood, coal, and other fuel sources accumulate in the home and are regularly inhaled contributing to asthma.
An asthma sufferer feels severe dyspnea (labored breathing) and wheezing. During an asthma attack, the bronchi become inflamed with eosinophils (white blood cells that promote inflammation) and mucus begins to build up. The bronchi smooth muscle hypertrophy (increase in size) and increase muscular activity causing intermittent obstruction of the bronchi.32 As they suffer to force air into the lungs, an asthma sufferer exerts more energy to overcome the constriction in the bronchi. According to the Equation 1, when resistance increases in the bronchi, flow in the bronchial passage diminishes. Asthmatics try to overcome this restriction by increasing their respiratory effort which directly influences ∆P. In reference to lung volumes (Figure 1), asthmatics have a decreased FEV (forced expiratory volume) to FVC (forced volume capacity) ratio and lower vital capacity since asthmatics are unable to move air into the deeper areas of the lungs. Furthermore, compliance in the lung decreases meaning that the elastic ability of the lungs to inflate and deflate are diminished.33 To counter this effect, inhalers with bronchodilators and corticosteroids help to reduce inflammation and open the air passages and decrease airway resistance.34
Air Pollution and Restrictive Lung Disease
Similar to obstructive pulmonary disease, restrictive lung disease prevents the filling of lung tissue. Specifically, it is a pulmonary disease that causes inflammation and fibrosis (thickening or scarring) of the lung interstitial tissue. Interstitial tissue of the lungs includes the lining of the alveoli. Restrictive Pulmonary Disease causes dyspnea, inspiratory crackling sounds, reduced lung volumes, and reduced lung compliance.35 Conditions like Coal Miner’s Lung, Silicosis, and Asbestosis are specific forms of pneumoconiosis. The term pneumoconiosis is a group of diseases related to the inhalation of small particulate matter to diseased states after a long period of exposure. Typically, these diseases develop in people whose occupation exposes them to environments where the air is filled with dust. Historically, these occupations were stone masons in Egypt. There, workers toiled in desert sands mining and carving giant blocks of stone while inhaling the dust from the stone. Throughout the Industrial Revolutions in England and the United States, workers crowded to big cities and were engulfed by air qualities so poor that many died of lung diseases. Today, industry is more regulated for air pollutants but, workers still face the same issues that their ancestors faced. An example of a restrictive pulmonary disease that continues to affect workers is Silicosis.
Silicosis the most prevalent occupational disease in the world. The condition occurs when workers inhale crystalline silica dust. The silica interacts with epithelial cells and macrophages and create nodules in the lung tissue. In the early stages of the disease, workers do not experience any shortness of breath, but in later stages the nodules become larger causing pulmonary hypertension, chronic hypoxia, and overall pulmonary dysfunction. Because of the disease also causes decreased macrophage count and decreased cell-mediated immunity response, a person with silicosis becomes more susceptible to other diseases like tuberculosis.36
Silicosis is caused by dust containing crystalline silica. This mineral can be found in mines, foundries, blasting operations, stone, clay, and glass manufacturing. The silica dust enters the respiratory passages and causes microscopic scar tissue to develop preventing the alveolus from exchanging gases. Patients experience shortness of breath, loss of appetite, chest pains, and respiratory failure. Though few actually die from silicosis, patients become more susceptible to other respiratory disease like tuberculosis according to the National Institute for Occupational Disorders.37
Second Hand Smoke and Electronic Cigarettes
Health concerns regarding second hand smoke have been a focus due to the tobacco-use cessation programs over the last thirty years. Unfortunately, the EPA estimates that 600,000 people die of second hand smoke inhalation each year and 40% of children worldwide have been exposed to environmental tobacco smoke.38 Though tobacco smoking has decreased, in many schools, including Mt. Pleasant High School the prevalence of electronic cigarettes (e-cigarette) and vaping (e-cigarette smoking) is on the rise. Instead of tobacco, an electronic includes a battery, an atomizer (heating element), and cartridge which contains the nicotine containing e-liquid (a mixture of nicotine and propylene glycol). The difference between traditional cigarettes and e-cigarettes is that the user is not exposed to tobacco combustion toxins and other carcinogens during inhalation. Though manufacturers of e-cigarettes initially meant them to help curb nicotine use, e-cigarette popularity is increasing worldwide.
A report by Callahan-Lyon showed that due to limited scientific research available the human health effects of electronic cigarette’ vapor are inconclusive. Her review does cite that residue from e-cigarette cartridges (e-liquid) can remain on surfaces for weeks. When chemicals like tobacco-specific nitrosamine (TSNA) mix with nitrous oxide, non-users may become exposed to carcinogens through inhalation, skin contact, or accidental ingestion.39 TSNA is a carcinogenic chemical found in tobacco products. Since many cartridges are flavored with sweet flavors, children can mistake the e-liquid as liquid candy. These flavors include vanilla, strawberry, cantaloupe, chocolate flavored e-liquids. Exposure to aerosol from exhaled e-cigarettes is less harmful than from tobacco second hand cigarette smoke. Despite the lower levels of aerosolized TSNA, Callahan-Lyon finds that residues of nicotine remain on surfaces for longer periods of time thereby increasing exposure through dermal contact, lung inhalation, and ingestion. Czogala et al. supports Callahan-Lyon’s results stating that exhaled vapor from e-cigarette users do expose non-users to nicotine. However the amount of nicotine exhaled is significantly lower than regular cigarettes. Their study compared different brands of e-cigarettes and showed that they do emit significant amounts of nicotine, but did not emit significant amount of carbon dioxide and volatile organic compounds, which is found in traditional tobacco smoke. As of 2013, very little research had been done to show the correlation of e-cigarette vapors and the health of the most vulnerable population: women, children, and those with pre-existing health conditions.40 Their findings represent an ambiguity that many students and tobacco users must decipher for themselves. Are e-cigarettes bad for you? Or is it still a better alternative to traditional cigarettes. Though the question can be argued for both sides (for now), it still stands that nicotine, whether inhaled or in contact with the skin, should be avoided especially by children where high levels of nicotine contact can lead to systemic toxicity. And, it is known fact that second hand smoke can lead to COPD, whether it is bronchitis or asthma. Furthermore, studies do show that vaping tends to lead to other tobacco use among teens who use e-cigarettes.41 Further study and investigation will surely change people’s perspective as to the safety of this currently poorly regulated product.

Comments: