Background
The Circulatory System
The Circulatory System consists of the heart and the arterial and venous system. In order to understand the organization it is necessary to discuss the anatomy of the heart and the anatomy of the arteries and veins. It is also important to trace the path of blood as it circulates through the body.
The Heart
The human heart is a four chambered pump. The pumping action of the heart is driven by the pacemaker (S-A node) which acts as a pulse generator that activates the muscles of the heart to contract. It is the changes in pressure within the chambers and the forceful contractions of cardiac muscle cells—collectively known as myocardium—that expels blood from the heart to the body. The heart includes two upper chambers called the atria and two lower larger chambers called the ventricles. The right and left ventricles are separated by a thick muscular wall called the interventricular septum. 5 The left atria and the left ventricle are separated by a valve, which opens in one direction to allow blood flow (from atrium to ventricle) but to prevent backflow. This valve is known as the bicuspid valve. Between the right atria and left ventricle is the tricuspid valve, which has a similar function. These valves open when pressure changes in the chambers and are aided by the chordae tendinae that are pulled by the contraction of the papillary muscles. Looking at the bisected heart macroscopically it is evident that the musculature of the left ventricle is far thicker than those surrounding the right ventricle and the atria above. 6 This is a key observation, since the left ventricle is the source of oxygenated blood that will be delivered to distance parts of the body, whereas the right ventricle sends blood to the lungs, which are nearby. The thickness of the muscular wall is related to the magnitude of the pressure that must be generated to drive blood through these different circuits.
Arteries and Veins
The arteries and veins differ in both structure and function. The arteries are subjected to the high blood pressures from the heart while the veins are not. Furthermore, the arteries function to deliver oxygen-rich blood to tissues of the body while veins function to return oxygen-poor blood to the heart. The aorta and pulmonary artery are two large arterial vessels stemming from the heart. In looking at the anatomy of the vessels further differences can be observed. The arteries and veins each have three major layers, the tunica interna, tunica media, and the tunica externa, however the veins have a thinner tunica media (a muscular layer) than the arterial vessels. 7 The reason for this difference is that arteries are subjected to high pressures against its walls, thus needing the resistance capability to withstand the stress of blood flow against its walls. Veins, on the other hand, are subjected to relatively low pressures. In addition, arteries need an ability to change their diameter, in order to regulate rates of blood delivery to the tissues that they serve. A thick muscular layer allows the arteries to control their diameter.
The veins have an added difference, in that many contain valves. These valves serve the purpose of preventing backflow of deoxygenated blood as it travels back to the heart. Like arteries, veins vary in size depending on the volume of blood they handle and location in the body. In general veins are larger in diameter than arteries increasing their capacity for blood storage. In this way, veins can serve as a blood reservoir. The superior vena cava and inferior vena cava are two of the largest veins entering the heart bringing de-oxygenated blood. 8
Blood
Blood is an organ comprised of various elements. Its composition is 55% plasma and 45% hematocrit or formed elements. The major elements include red blood cells (erythrocytes), white blood cells (leukocytes), and platelets, which are suspended in a matrix called plasma. 9 Red blood cells are biconcave discs increasing their ability to take up oxygen and bind hemoglobin. As red cells move through the arteries and veins they have the ability to fold or inflate. White blood cells are classified into granulocytes and agranulocytes depending on the presence of granules in the cytoplasm. Unlike red blood cells, the main purpose of white blood cells is defense; they respond to injury and the presence of foreign cells. Plasma is the fluid which all formed elements of blood travel through. Because plasma is 91% water it's a low viscosity fluid making it ideal for the formed elements to travel through. 1 0
Blood Flow
Systemic Circuit
The circulatory system serves as the highways for blood to travel through. It can be divided into major highways of functional blood flow - the systemic circuit and pulmonary circuit. The systemic circuit includes the heart, arteries, capillaries, and veins that deliver oxygenated blood to the tissues of the body. (Fig. 1 1 1) The path of blood can be traced in a circular pattern beginning at any point in the body. Beginning in the left ventricle of the heart blood passes through the aortic valve, through the aorta, and into the systemic circulation. The large arteries bifurcate into smaller arteries. As the arteries become smaller in diameter they become arterioles which lead to capillary beds - the site of oxygen / carbon dioxide exchange. As oxygen diffuses into the tissues, carbon dioxide begins its path to the lungs for expulsion and de-oxygenated red blood cells return to the heart for re-oxygenation. Capillary beds lead to small venules and larger veins, ending with the superior and inferior vena cava. De-oxygenated blood is dumped into right atrium and passes through the tricuspid valve into the right ventricle. 1 2
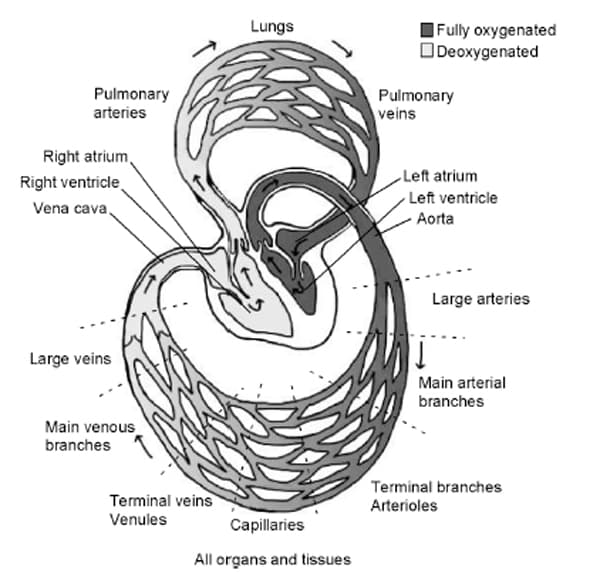
Fig. 1. The path of blood through the circulatory system. Image reproduced from Saltzman (2009) with permission.
Pulmonary Circuit
The pulmonary circuit of blood flow includes the heart and the lungs. Its major function is to deliver de-oxygenated blood to the alveoli, deep in the lungs, and to return oxygenated blood to the left side of the heart. Blood from the systemic circuit leaves the right atrium through the pulmonary valve and pulmonary artery. Once carbon dioxide/oxygen exchange is achieved, pulmonary veins return oxygenated blood to the left atrium of the heart. At this point oxygen rich blood is ready again to enter the left ventricle through the biscuspid valve for systemic circulation.
Blood Pressure and Hypertension
In surveying my students, many are familiar with the idea of blood pressure but are not aware of the multiple health implications of untreated hypertension. Furthermore, though the term "pressure" is understood, they do not understand where the pressure exists or what it is pressing against. I plan to delve deeper into the topic of hypertension, with a focus on minority populations, so that the subject becomes more relevant to my students' lives. Over the course of the unit it is my hope that students will gain a fuller understanding of the circulatory system and how "the silent-killer" known as hypertension can affect on the human body if left untreated.
Pressure & the Cardiac Cycle
The idea of pressure seems easy enough to understand if one were asked to apply pressure on a wound. The word implies a force and pressure is a measure of force against a specific surface area. Atmospheric pressure is the amount of force per unit area exerted against a surface by the weight of air above that surface in the Earth's atmosphere. In order to measure pressure, we use manometers with fluids inside like mercury (Hg), since we know the mass of mercury, we can track the amount of mercury displaced as a measurement of pressure. Thus, mm Hg, means the amount of force exerted to move mercury x amount of Hg some mm. When the force (i.e. pushing) is increased then the pressure against the specific surface area also increases. Pressure is measured in mm Hg because at sea level, the atmosphere or air around us can support a 760-mm column of mercury inside a glass tube called a barometer. The pressure (P) exerted by a column of liquid of height h and density Ρ is given by the hydrostatic pressure equation: P = Ρgh. In measuring blood we use as device called a sphygmomanometer, which is a type of manometer used with an inflatable arm cuff to measure blood pressure. When taking one's blood measure we are measuring the amount of pressure required to block circulation to the artery and then the amount of pressure that blood within the vessels exerts against the pressure from the cuff. Thus, the systolic and diastolic pressure are in units of mm Hg.
The Cardiac Cycle
Though students have often heard of the words systolic and diastolic pressure, they often cannot relate it to the actual events in the cardiac cycle nor are they aware of the mechanics of a blood measure monitor.
In the cardiac cycle, pressure and blood volume can be tracked in order to understand how blood pressure and myocardial contraction/relaxation are related. Pressure gradients (differences in pressure between different locations) and strength of myocardial contraction drive the flow of blood. Atrial contraction pushes blood into the ventricles because the pressure in the atria is higher forcing the tricuspid and bicuspid valves to open, allowing the ventricles to fill. The increase in pressure of the atria is due to the pressure exerted by blood as it fills the atria. The time during which the atria contract is called atrial systole. As the ventricles fill, pressure changes and volume changes, the atrioventricular valves (tricuspid and bicuspid valves) close at the point in which ventricular pressure is higher than atrial pressure. As the ventricles continue to contract (ventricular systole), the increasing pressure on the blood volume forces a ventricular ejection. Blood from the left ventricle is expelled into the aorta when the aortic valves open, while blood in the right ventricle is expelled into the pulmonary artery when the pulmonary valves open. At this point aortic pressure is lower than ventricular pressure thus allowing the expulsion of blood from the ventricles. Because of the change in blood volume in the ventricles, the pressure changes once again causing the aortic and pulmonary valve to close and the ventricles to relax marking the beginning of ventricular diastole. Soon the atria will once again fill beginning the cycle once again. 1 3
When blood pressure is measured using a blood pressure monitor, it is the force that blood exerts against a point in the arteries that is measured. If a sphygmomanometer is used, it is used in conjunction with a stethoscope. The cuff is used to apply pressure around the arm, blocking blood flow in the brachial artery. As the pressure is slowly released the sound of blood rushing through the occluded point is measured: this is the systolic pressure that is first recorded. When the sound of blood movement is no longer heard, the pressure is recorded as diastolic pressure. 1 4
Regulation of Blood Pressure
Normal blood pressure is 120 mm Hg/ 80 mm Hg (systolic/diastolic). Though this mean arterial blood pressure is commonly known in adults, what is not commonly known is that pressure varies throughout the whole circulatory system. Because of these changes, pressure drops create a means through which blood can circulate. However, how fast or slow blood circulates is not only determined by the amount of pressure drops in the arteries and veins. Recalling that blood pressure is the force against the arterial walls, it is subjected to various factors that change the initial force. Such factors include viscosity of blood, the peripheral resistance of arteries, and the distance from the original source of the force. Changes to the viscosity of blood and the resistance of the arteries will cause an imbalance in the mean arterial pressure. Because the body likes to maintain a homeostatic balance, neural reflexes in conjunction with negative feedback loops take action to maintain the mean arterial pressure.
Neural Reflexes
The human body regulates itself through a series of mechanisms called negative feedback loops. A feedback loop includes a sensor or detector to a stimulus, a control center which makes decisions as to how to respond to the stimulus, and an effector which sends a resulting response to the stimulus. A simple example is the response the body would have to changes in temperature. If sensors within the skin detect a drop in temperature, they will send signals to the brain to send the appropriate response to the muscles in the skin to contract. One effect of the stimulus is the contraction of arrector pili muscle to raise the hair on your skin causing goose bumps. Another is to stimulate skeletal muscles to contract (shiver) causing you to generate heat, which is a byproduct of skeletal muscle contraction. 1 5 In a similar fashion negative feedback loops regulate arterial blood pressure. This reflex involves a detector, afferent neural pathway, coordinating center in the brain, efferent neural pathway, and effectors. Primary receptors include baroreceptors which are stretch receptors in the vascular walls and secondary receptors include chemoreceptors in blood. The medulla is the coordinating center which makes the decision as to how to respond to the detectors. The effectors are the heart pacemaker (the SA node), cardiac muscle, vascular smooth muscle, and adrenal medulla that ultimately carry out the action in the organ. 1 6
Baroreceptor control of arterial pressure is a type of feedback loop that includes a detector (baroreceptor), an afferent neural pathway, a control center (medulla), and an efferent neural pathway that activates the effectors (heart and blood vessels). Baroreceptors are located in high pressures areas of the carotid sinus and aortic arch. 1 7 Because baroreceptors are stretch receptors they do not really respond to high pressure within arteries, they are instead responding to the stretching of the arterial wall due to high pressure or increased intravascular volume. The more the arterial wall stretches, the more the afferent neurons fire nerve impulses to the medulla. The medullary cardiovascular center is responsible for deciding which type of response is appropriate. The response will either be acceleratory or inhibitory. If the response is to accelerate heart rate then sympathetic nerve fibers will be fired. The result will be an increase in heart rate. If the response is to inhibit or to slow heart rate and thereby decrease pressure, parasympathetic efferent fibers will fire. The result of parasympathetic nerves firing is decreased heart rate, reduction in cardiac contraction, and vasodilatation, thus reducing mean arterial blood pressure. 1 8
Peripheral Resistance
Besides neural reflexes, peripheral resistance is a factor that affects blood flow. Resistance depends on the thickness of the fluid (viscosity) and the structure of the vessels through which it flows. (Fig. 2) It is the frictional force of blood against the walls of the blood vessels. Thus when there is more resistance, the heart will have to pump harder to overcome that force. Blood viscosity is the ease with which blood flows through the vessels. Thus the more viscous blood is blood pressure rises since the heart will have to work harder to move that same volume of blood with its increased blood cells and blood proteins. 1 9
Fig. 2 Resistance Equation 2 0
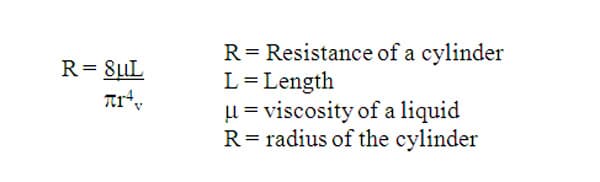
In addition, peripheral resistance is yet another factor that alters flow. At a given pressure gradient, peripheral resistance decreases blood flow: when the flow must be maintained constant, an increased resistant requires an increase in blood pressure. However, peripheral resistance can be overcome by changing the diameter of the blood vessel. Vasodilation decreases resistance by increasing the diameter through which blood can flow through a certain point. Vasoconstriction has the opposite affect which increases resistance by decreasing the diameter through which blood can flow. The vasomotor center of the brain is responsible for controlling the muscle of arterioles. Sending sympathetic impulses causes vasoconstriction and thus an increase in peripheral resistance and blood pressure. While decreasing the sympathetic impulses has the opposite effect. 2 1
Hypertension
Hypertension is the state at which arterial blood pressure is consistently elevated above the normal pressure of 120 mmHg over 80 mmHg. A person who is hypertensive would have a systolic pressure greater than 139 mmHg and a diastolic pressure greater than 89 mmHg.
There are various stages of hypertension: Prehypertension, Stage 1, and Stage 2. Pre-hypertension describe a slight rise in normal or ideal pressure. The systolic rate would have to between 120 and 139 mmHg, while the diastolic would be between 80 to 89 mmHg. Stage 1 Hypertension would be a systolic rate above 140 mmHg and 80 mmHg for the diastolic rate. Stage 2 hypertension is indicated by a blood pressure or 160/100 mmHg. In addition there are different types of hypertension: primary hypertension and resistant hypertension. Primary hypertension usually develops as one ages. Resistant hypertension may be due failure of someone with hypertension to ignore their condition or they have become resistant to prescriptions for lowering blood pressure. 2 2
Treatments
Treatments for people with hypertension vary from simple changes of diet and exercise, to pills, to implantable devices. The prescribed medical treatments available for patients who are hypertensive include various medications including diuretics (or water pills), beta blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and direct vasodilators. If the hypertension is resistant to medications, implantable baroreflex hypertension systems like Rheos System are available. This implantable device is designed to regulate pressure sensors in the brain and thereby trigger effectors in the body that effectively lower blood pressure.
The use of baroreflex stimulation began as early as the 1950s in hypertensive dogs. Later applications by Carlsen and colleagues led to successful results in reducing hypertension in a 40 year old man with long-standing history of hypertension and regular use of four anti-hypertensive drugs. With treatment, his BP fell from a 250/195 to 150/90 mm Hg. Implantable devices were slow to develop due to limitations in technology, thus clinical use of activating baroreceptors to reduce blood pressure was impeded. 2 3
Currently the Rheos Hypertension System® by CVRx is in clinical trials, and it shows great promise in reducing mean arterial blood pressure. The baroreflex hypertension therapy includes three components an Implantable Pulse Generator, Carotid Sinus Leads, and external Programmer System. The small cell phone sized pulse generator is surgically implanted beneath the collar bone and under the skin. The carotid sinus leads are attached to the carotid arteries on both sides of the neck. Finally, the programmer system is external so the frequencies of the pulses that stimulate the baroreflex are adjusted specifically for each patient. 2 4 Clinical studies reported in Current Hypertension have shown great promise for the Rheos system, showing marked decreases in resistant hypertensive patients. After 3 years, under BHT therapy, patients have shown up to a 30 mm Hg drop in systolic pressure for those having a systolic pressure of 190 mm Hg. While diastolic pressures have been shown to drop 22 mm Hg for those with diastolic pressure of 112 mm Hg. 2 5 Besides the reduction in blood pressure, Bisognano and Kaufman have shown an improved cardiac structure with baroreflex activation therapy. Using the Rheos system they report improved ventricular function and size. 2 6 Because of the success of the Rheos System, its use may eventually expand to a heart failure treatment.
Another technological advancement that may help patients who have irreparably damaged blood vessels is tissue-engineered vascular grafts. 2 7 Dr. Laura Niklason and her groups of research scientists have developed a technique that allows vascular tissues to be grown in laboratory bioreactors. Their process involves using donor smooth muscle cells that are grown on polyglycolic acid (PGA) scaffolds shaped like a vessel. Within a bioreactor containing media that allows for optimal tissue growth, the smooth cells proliferate and invade the PGA scaffold. Over a period of time, enough cells accumulate on the scaffold that assumes the shape of the vascular tube. When the PGA degrades and is dissolves away, the remaining tissue is a vascular graft. 2 8 Thus far, the tissue is used as a dialysis graft, showing great potential because of its durability and lack of immunological rejection. This technology is especially interesting for hypertensive patients since the engineered vascular graft is able to resist high pressures up to 2150 mmHg whereas native tissues can withstand pressures up to 1680 mm Hg. 2 9 Tissue engineered arteries may soon be able to replace atherosclerotic vessels in addition to its current use as a dialysis graft.
Cardiovascular Disease
Because high blood pressure and hypertension can lead to serious cardiovascular disease, it is important to introduce the concept. Cardiovascular disease (CVD) can include any disease that can affect your heart and the blood vessels. Included is a long list of heart related disorders like arrhythmias, coronary artery disease, heart infections, and congenital heart defects. A person with arrhythmias may experience symptoms of tachycardia (fast heartbeat), bradycardia (slow heartbeat), chest pain, dizziness, and shortness of breath. People with heart defects may have blue skin due to lack of oxygen circulating, shortness of breath, and swelling in the extremities. Another form of CVD called cardiomyopathy causes sensations of fatigue, breathlessness, irregular heartbeat, and swelling due to the thickening or stiffening of the cardiac muscle. Problems with the valves of the heart include symptoms of chest pain, shortness of breath, heart murmurs, and fainting. All of the above are examples of cardiovascular disease. 3 0
Coronary Artery Disease
Coronary Artery Disease (CAD) is the gradual blockage of the coronary arteries of the heart due to atherosclerosis. As plaque builds up within the small arteries, the lumen begins to narrow and flow of blood eventually slows or stops. People with CAD may experience angina (chest pain), breathlessness, fatigue, and weakness. Often patients with CAD are on blood pressure medications to lower their blood pressure. Some may take nitroglycerin pills to decrease chest pain. 3 1

Comments: